CUHK Introduces Asia's First "Gastric Pacemaker" To Restore Digestive Function in Gastroparesis Patients
The Faculty of Medicine at The Chinese University of Hong Kong (CUHK) has successfully completed Asia’s first “Gastric Pacemaker” implant surgery in March 2014. The patient concerned has been suffering from gastroparesis for sixteen years whose daily lives were seriously affected. After the treatment, the patient’s digestive function has been restored. As gastroparesis is a chronic condition that cannot be cured, the innovative “Gastric Pacemaker” has brought new hope for the treatment of the chronic condition.
On average, one in every ten people in Hong Kong is suffering from functional disorders of the stomach. Among them, 20-30% are diagnosed as “Gastroparesis”, a condition in which the stomach cannot empty food properly.
Normally, the stomach expands to hold food and contracts to move food down the small intestine for further digestion. Gastroparesis is a medical condition arising from paresis of the stomach, causing difficulties for food to move through the digestive tract. The patients’ appetite will be affected as they will feel full quickly. Symptoms include abdominal pain, heartburn, abdominal bloating and a constant feeling of fullness, affecting the daily lives of the patients.
Similar to a “Cardiac Pacemaker”, the six-centimeter-long “Gastric Pacemaker” implanted in the patient’s body through minimally invasive surgery will help restore the motion of the stomach by gastric electrical stimulation. The patient can resume normal diet as the digestive system resumes its normal functioning.
Professor CHIU Wai Yan, Philip, Assistant Dean (External Affairs) of the Faculty of Medicine and Director of the CUHK Jockey Club Minimally Invasive Surgical Skills Centre, who was responsible for this operation, said, “The operation lasted for over 100 minutes. This is the first trial in Asia, representing a major breakthrough in the treatment of Gastroparesis in the region. Gastroparesis is a debilitating condition that can lead to severe disturbance in eating as well as daily activities. We are happy to learn that our patient had gained 5 pounds in half year’s time after the surgery."
The current first-line controller drugs for functional disorders of the stomach can only help relieve the symptoms and mitigate the influence on the patients’ daily lives. However, the medication may not be effective on every patient. The introduction of “Gastric Pacemaker” has brought new hope to these patients.
The causes of stomach disorders are yet to be known. Some gastrointestinal diseases, such as stomach cancer, esophageal cancer, gastric ulcer, may trigger the same symptoms, making stomach disorders difficult to be diagnosed. Patients have to undergo thorough upper gastrointestinal endoscopy test to eliminate the possibility of having other serious diseases.
Professor WU Che Yuen, Justin, Associate Dean (Development) of the Faculty of Medicine and Director of the S.H. Ho Centre for Digestive Health said, "Patients with functional disorders of the stomach generally appears to be healthy. The symptoms may be caused by poor dietary habits, stress, sleep disorders or emotional factors. The patients may get worse when under stress or having emotional problems. We will advise them to modify their diet and daily habits, avoid eating too much or too fast, so as to help alleviate the condition."
The introduction of “Gastric Pacemaker” showcases how the advancement of innovative medicine can benefit patients, as well as the community at large. To gather the resources to promote innovative research and development of clinical practice, Chow Yuk Ho Technology Centre for Innovative Medicine will be established early next year, working closely with the Faculty of Engineering at CUHK to develop more innovative medicines and treatments.

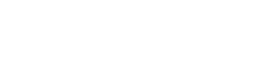
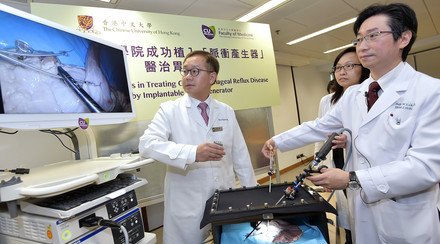
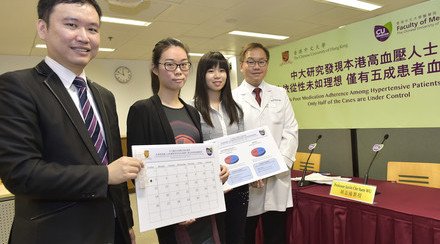
The patient who underwent Asia’s first “Gastric Pacemaker” implant surgery, Chan Chi-kit (middle), and the responsible doctors - Professor CHIU Wai Yan Philip (right), Assistant Dean (External Affairs) of the Faculty of Medicine and Director of the CUHK Jockey Club Minimally Invasive Surgical Skills Centre, and Professor WU Che Yuen Justin (left), Associate Dean (Development) of the Faculty of Medicine and Director of the S.H. Ho Centre for Digestive Health – pose for a group photo. On Professor Chiu’s and Professor Wu’s hands are the six-centimetre-long “Gastric Pacemaker” and monitor instrument respectively.

Professor Philip Chiu (right) demonstrates the laparoscopic implantation of a “Gastric Pacemaker”, which can help gastroparesis patients to restore stomach function by gastric electrical stimulation. The patient can resume normal diet as the digestive system restore its normal functioning.

Chan Chi-kit (right), 23-year-old, has been suffering from gastroparesis for sixteen years whose daily lives had been seriously affected. After the treatment, his digestive function has been restored.