Multicomponent Frailty Prevention Programme Reduces Frailty Over 80% of Pre-frail Elderly Reverse to Robust Phenotype
A recent study conducted by the Department of Medicine and Therapeutics of the Faculty of Medicine of The Chinese University of Hong Kong (CUHK) and CUHK Jockey Club Institute of Ageing proved the effectiveness of a multicomponent frailty prevention programme (the Programme) in improving physical and cognitive functions, and self-rated health in pre-frail community-dwelling older persons in Hong Kong.
CUHK Faculty of Medicine collaborated with Jockey Club CADENZA Hub to conduct the study on the Programme. The study showed that participation in exercise, cognitive training and board game activities, had decreased the combined assessment of frailty score significantly in the intervention group, but that it had increased in the control group. In addition, over 80% of the older persons in the intervention group have reversed from “pre-frailty” to “robust” phenotype. The findings have been published in the Journal of the American Medical Directors Association.

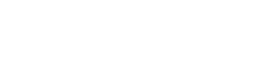
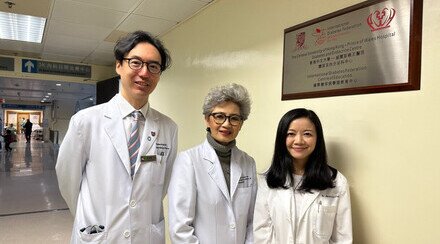
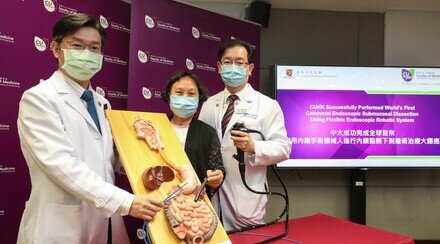
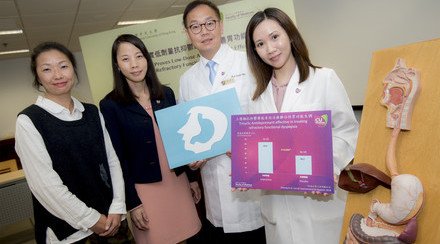
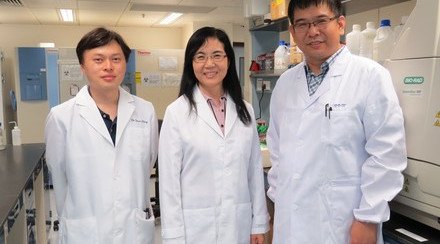
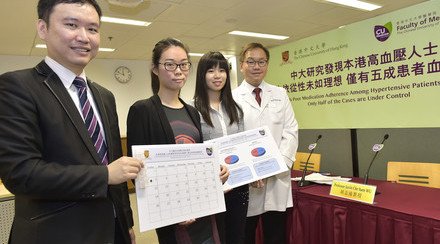
A recent study conducted by CUHK proves the effectiveness of a multicomponent frailty prevention programme in improving physical and cognitive functions, and self-rated health in pre-frail community-dwelling older persons in Hong Kong. Over 80% of the older persons in the intervention group have reversed from “pre-frailty” to “robust” phenotype. (From right) Dr. Ruby YU, Senior Research Fellow of the Department of Medicine and Therapeutics of the Faculty of Medicine at CUHK and CUHK Jockey Club Institute of Ageing; Prof. Jean WOO, Research Professor of the Department and Director of the Institute; Anna, participant of the study; and Ms Jenny CHENG, Senior Nursing Officer of the Jockey Club CADENZA Hub.
Over 60% of Hong Kong adults aged 65 or above are “pre-frail” or “frail”
Frailty is a geriatric syndrome resulting from psychological and multisystem physiological declines in reserves. In Hong Kong, over 60% of adults aged 65 or above are classified as “pre-frail” or “frail”. Older people living with frailty are more vulnerable to deterioration and negative health outcomes such as increased risk of falls, disability, hospitalisation, institutionalisation, or even death. Furthermore, a recent analysis of data from multiple birth cohorts found that older people today are experiencing their later years with higher levels of frailty than their counterparts of previous generations. With an ageing population, the number of older people with frailty is expected to increase.
Professor Jean WOO, Professor of the Department of Medicine and Therapeutics of the Faculty of Medicine and Director of CUHK Jockey Club Institute of Ageing, explained, “In view of the ageing population, strategies that can help prevent or delay the onset of frailty are important. Frailty prevention trainings can be developed and implemented in community elderly centres to reduce frailty in the community.”

Prof. Jean WOO (left) states that strategies which can help prevent or delay the onset of frailty are important in an ageing population. Frailty prevention trainings can be developed and implemented in community elderly centres to reduce frailty in the community.

Anna (left) says that her physical and cognitive functions have been improved after participating the multicomponent frailty prevention programme. Her muscle has increased and she does not feel short-of-breathe easily when climbing inclined road.
Combined frailty score was reduced by 36% in the intervention group
From 2017 to 2018, 127 “pre-frail” participants from community elderly centres of Hong Kong, with mean age of 62.2 years, were randomly assigned to an intervention group or to a control group. The intervention was a multicomponent frailty prevention programme consist of aerobic and resistance exercises, computer-assisted cognitive training, and board game activities that were carried out twice a week for 12 weeks. The primary outcomes were frailty status and a combined frailty measure including subjective (frailty status) and objective (grip strength, muscle endurance, balance, gait speed) measures. The secondary outcomes were attention, memory, executive function and self-rated health.
Participants were assessed by answering 5 yes-no questions, and be categorised as “robust” (0 point), “pre-frail” (1-2 point) or “frail” (3-5 point). The results of the intervention group and the control group at week 12 are as follows:
Intervention Group | Control Group | |
Participants reversed from “pre-frailty” to “robust” phenotype | 83.3% | 1.6% |
Participants with low muscle endurance | Reduced 70.8% | Increased 28.6% |
Participants with poor balance | Reduced 89.5% | Reduced 17.6% |
Combined assessment of frailty score | Reduced 36.4% | Increased 3.1% |
In addition, participants in the intervention group had greater improvements in cognitive functions and self-rated health than in the control group. Details are tabulated as below:
Intervention Group | Control Group | |
Attention and memory (digit span score) | Increased 4.8% | Reduced 1.4% |
Executive function (frontal assessment battery score) | Increased 13.8% | No changes |
Participants with self-rated health as “Poor or fair” | Reduced 34.8% | Reduced 8.2% |
Dr. Ruby YU, Senior Research Fellow of the Department of Medicine and Therapeutics and CUHK Jockey Club Institute of Ageing, stated, “The multicomponent frailty prevention programme reduced frailty and improved physical and cognitive functions, and self-rated health in pre-frail community-dwelling older persons. Findings of the study encourage promotion and implementation of the multicomponent frailty prevention programme in the welfare sector or delay progression of frailty in older people.”
For more information about the study, please browse: