CUHK Launches Hong Kong’s First Pilot Integrative Medicine Programme in Multiple Sclerosis for Managing Cognitive Symptoms, Relieving Fatigue, and Disease Control
The first integrative medicine pilot programme for multiple sclerosis patients in Hong Kong is about to be launched by The Chinese University of Hong Kong’s (CUHK) Hong Kong Institute of Integrative Medicine (HKIIM). Under the programme, patients will receive western medications, Chinese herbal therapy and acupuncture under the close supervision and care of the clinical team. The objective of the programme is disease control, at the same time managing patients’ cognitive symptoms and fatigue and thereby restoring mobility.
MS Prevalence rate has risen by 40% in seven years
Multiple sclerosis (MS) is affecting an estimated 2.5 million young adults worldwide. According to the latest figures of the Hong Kong Multiple Sclerosis Registry of CUHK, the prevalence rate of MS is mounting, from 4.8 per 100,000 people in 2008 to 6.8 per 100,000 people in 2015. In Hong Kong, more than 500 people have been diagnosed with MS. The age of onset is between 20 and 30 years, and more than 70% are female.
MS is the most common central nervous system demyelinating disease. Its exact etiology remains unknown. The disease occurs when the insulating covers of nerve cells in the brain and spinal cord are damaged, affecting the functions of the optic nerve, brain, brainstem, cerebellum or spinal cord. Once the nerve fails to transmit signals properly, the respective functions will be disrupted. That results in a wide range of signs and symptoms, including blurred vision, muscle weakness, memory loss, and bladder difficulties.
Managing MS symptoms with Western and Chinese medications
Most patients develop a relapsing-remitting course in the beginning and if they fail to receive timely treatment, the recurrent damage may eventually lead to disability. Interferon is commonly used as the first-line treatment in Hong Kong, nowadays. Researches suggest that early stage disease is most responsive to disease modifying treatments, which can significantly reduce the relapse rate (by 30%) and long term disability. However, newer agents such as oral medications and infusion biologics, can additionally prevent relapses (>50%), reduce MRI lesions and progression, and have a higher chance of achieving ‘disease-freedom’, or ‘no evidence of disease activity’ – which is considered a new benchmark of disease control. Nevertheless, fatigue (>80%) and cognitive symptoms (40-60%) are prevalent among MS patients and difficult to treat.. The physical impairment disables patients’ mobility, problem-solving skills and self-care ability, resulting in a poorer quality of life.
To address and solve that unmet need, HKIIM has been, since August 2014, exploring options offered by Integrative Medicine (IM) in treating these important symptoms of MS by close collaboration between neurologists and Chinese medicine practitioners (CMPs). Dr. Alexander Yuk Lun LAU, Assistant Professor, Department of Medicine and Therapeutics and Deputy Chief Clinician of Integrative Medical Centre, Faculty of Medicine said, ‘Per our discussion with CMPs, Chinese herbal medicine and acupuncture are found efficacious in resolving MS symptoms. We have thus started exploring how western clinicians and CMPs may collaborate on the diagnosis, assessment, monitoring and treatment of MS.’
Mr. William Hoi Ngai CHEUNG, Professional Consultant, HKIIM and Deputy Chief CMP of the Integrative Medical Centre, Faculty of Medicine, explained, ‘MS is a disorder of the brain and spinal cord. Traditional Chinese Medicine views the kidneys as the center of the body's “yin” and “yang”. Kidneys store yin-essence in order to produce marrow to enrich the brain, therefore in the Chinese medicine perspective, MS is associated with a “kidney deficiency”. Patients often demonstrate symptoms of lower limbs weakness, dizziness and insomnia at an early stage. When the disease evolves into a chronic progressive phase, patients may suffer from listlessness, fatigue and heavy limbs, or even cold limbs and waist. Paraplegia may result in some severe cases. On the basis of the syndrome differentiation of the MS patients, CMPs may then prescribe suitable Chinese herbal formulae. Acupuncture is an effective treatment modality in mind-refreshing, dredging meridian, relieving numbness and improving coordination. Acupuncture can be used concomitantly to invigorate “qi”, so as to manage the symptoms of listless, muscle weakness and incontinence of some patients.’
Dr. Vincent Chi Ho CHUNG, Assistant Professor, School of Public Health and Primary Care and Associate Director (Education) of HKIIM stated that international studies also showed Chinese herbal medicine and acupuncture are efficacious therapies for the management of MS. A study found the disability score and the relapse rate in patients with MS improved after receiving Chinese herbal medicine. Another study also showed that acupuncture benefitted MS patients in reducing fatigue, pain and mood disturbances. There was also an improvement found in patients’ quality of life after treatment. Both studies concluded that no significant side effects were observed in patients who underwent Chinese herbal treatment and acupuncture.
Dr. Alexander Yuk Lun LAU continued, ‘There were 20 MS patients who had received IM care conjointly managed by neurologists, CMPs and nurses in our clinic. Initial findings showed an improvement in fatigue, numbness and cognitive functions. Our IM clinical team is going to launch a pilot programme for a hundred patients with confirmed relapsing multiple sclerosis. Selected patients will receive an 8-week IM treatment of herbs and/or acupuncture. This programme aims to evaluate the treatment outcome of the IM model in managing fatigue and cognitive symptoms associated with multiple sclerosis.’ Neurologists, CMPs and nurses will collaborate to assess and monitor patients’ health conditions. Clinical toxicologists will also be involved and render advice on herb-drug interactions. Dr. LAU remarked, ‘MS is most often diagnosed in young adults. If the IM approach is found to be efficacious in ameliorating the disturbing symptoms of fatigue and cognitive impairment, it might open up a novel therapeutic modality for MS. As such, patients would have chances to regain their strengths in recreation, daily routines and self-care.’
Prof. Justin Che Yuen WU, Associate Dean (Development), Faculty of Medicine and Director of HKIIM concluded, ‘Our integrative medicine models have three distinctive features. First, we have a designated team of western clinicians and CMPs who are responsible for the design and implementation of programmes. Second, the clinical team develops close and effective communications in the clinical setting. Third, the clinical team is dedicated to developing quality pragmatic clinical trials (original research), with an aim to evaluate the integrative medicine patient care model and treatment outcomes. We are dedicated to establishing a platform which respects and maximizes the individual strength of Western and Chinese medicine to precipitate the development of integrative medicine. If we achieve breakthrough results showing that integrative treatment could be a safe and more effective treatment modality in certain diseases, different areas of medical practice could be bridged and benefit the community as a whole.’
Established with funding from The Hong Kong Jockey Club Charities Trust, CUHK’s Hong Kong Institute of Integrative Medicine is the first of its kind in the city, incorporating Chinese and Western integrative medical treatment, education and research under one roof.
The Hong Kong Jockey Club Charities Trust has been a long-standing supporter of various projects that promotes the development of Chinese medicine in Hong Kong, and helps meet the needs of different patients and facilitate professional training. They include the establishment of traditional Chinese Medicine out-patient clinic and dispensary; and the set-up of a Chinese Herbs Garden. This integrative medicine pilot programme for multiple sclerosis patients is also supported by the Hong Kong Jockey Club Charities Trust. For participation or enquiry, please dial 2873-3100 or send email to hkiim@cuhk.edu.hk .

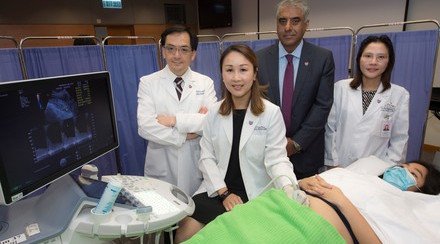
Prof. Justin WU (3rd left), Director of CUHK’s Hong Kong Institute of Integrative Medicine (HKIIM); Dr. Vincent CHUNG (1st left), Associate Director (Education) of HKIIM; Mr. William CHEUNG (4th right), Professional Consultant of HKIIM; Prof. Songming LIANG (3rd right), Honorary Visiting Professor of HKIIM; and Dr. Alexander LAU (4th from left), Deputy Chief Clinician of CUHK’s Integrative Medical Centre; introduce the pilot integrative medicine programme for multiple sclerosis patients to be launched by HKIIM.

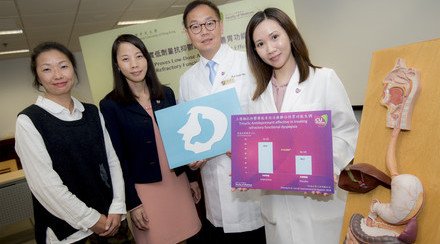
Multiple sclerosis patients Gary (2nd left) and Don (2nd right) have been suffering from associated symptoms since 2013 and 2014, respectively. Their symptoms are relieved after receiving Integrative Medicine treatment.

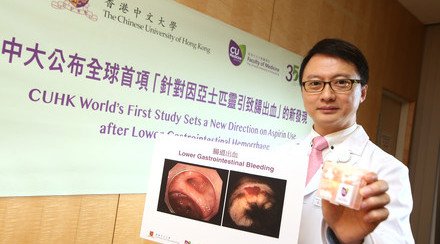
Dr. Alexander LAU states that the prevalence rate of multiple sclerosis in Hong Kong has been increased by more than 40% from 2008 to 2015.