CUHK
News Centre
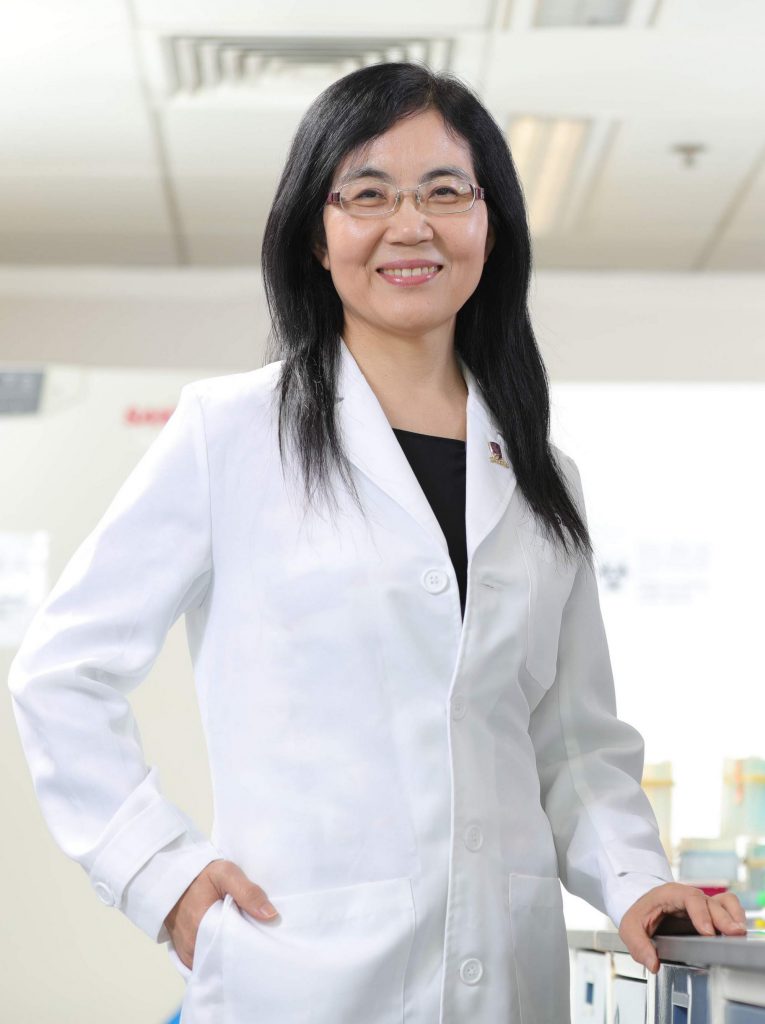
CUHK Professor Jun Yu and her team receive the State Natural Science Award second-class award
The research team led by Professor Jun YU from the Department of Medicine and Therapeutics, The Chinese University of Hong Kong (CUHK) was honoured with the State Natural Science Award (SNSA) second-class award for the project entitled “Integrative Research on Natural History, Mechanism, Potential Diagnostic and Therapeutic Targets for Non-alcoholic Fatty Liver Disease and its related Hepatocellular Carcinoma”. Members of the team also include Professor Vincent Wai Sun WONG, Professor Henry Lik Yuen CHAN, Professor Xiang ZHANG, and Professor Joseph Jao Yiu SUNG.
Non-alcoholic fatty liver disease (NAFLD) is caused by excessive fat accumulation in the liver. It is the most common chronic liver disease in the world, affecting 15%-40% of the global population. In China, the incidence of NAFLD has been rising rapidly due to the changes in lifestyle. NAFLD comprises a wide spectrum of liver diseases, ranging from simple steatosis to steatohepatitis (NASH), which can progress to liver fibrosis and eventually to hepatocellular carcinoma (HCC). For 18 years, Professor Jun Yu, Professor Vincent Wai Sun Wong and their team have achieved a series of major breakthroughs, which not only broadens the understanding of the occurrence, development process and high risk factors of NAFLD, but also elucidates the critical molecular mechanism of the development of NAFLD and its related HCC, followed by identification of potential therapeutic targets. More importantly, the findings of this project have thoroughly accelerated the development of prevention, non-invasive early diagnosis, assessment, and treatment for NAFLD, providing an unneglectable and solid step in overcoming NAFLD in the future. Altogether, this project has brought tremendous insights into basic and translational research on NAFLD.
The team is the first to systematically elucidate the key molecular mechanisms and clinically applicable therapeutic targets of the progression from simple steatosis to NASH/liver fibrosis.
The team discovered the key factors such as heme oxygenase (HO-1) and cytokine CXCL10/receptor CXCR3 in NASH/liver fibrosis, and their related molecular pathways and mechanisms. They also elucidated multiple effective treatments for NASH, including HO-1 agonist Hemin and CXCR3 antagonist AMG487. In addition, the team revealed that a Chinese medicine Phyllanthus urinaria could prevent NASH progression. These findings provide the fundamental for establishing novel preventive measures against NASH/liver fibrosis.
The team is the first to reveal the mechanism of NASH progression to NAFLD-related HCC, and discover their therapeutic targets.
The team identified numerous novel gene mutations in NAFLD-HCC by whole genome sequencing and functional experiments (such as mutation of cholesterol ester hydrolases CEL). They also deciphered that excess dietary intake of cholesterol could induce NAFLD-HCC development through promoting expressions of abnormal and mutated hepatic genes. For the first time, the team found that SQLE, a key rate-limiting enzyme for cholesterol synthesis, could induce NAFLD-HCC. They therefore proceeded with their investigation and revealed that the inhibitor of SQLE terbinafine is an effective drug against NAFLD-HCC.
The team successfully identified multiple diagnostic biomarkers, invented a clinical scoring system, and established a robust platform for non-invasive diagnosis of NASH/liver fibrosis.
Due to the high prevalence of NAFLD and the continual progression of NASH to liver fibrosis or even HCC, it is therefore important to perform non-invasive diagnosis at early disease stage. The team discovered several serum markers for diagnosing NASH such as CXCL10. They reported the application of transient elastography for non-invasive diagnosis of NASH/liver fibrosis. The team also established a predictive scoring model and system for assessing the disease stage of liver fibrosis in NAFLD patients.
The team has comprehensively reported the natural history of NAFLD and its associated risk factors, and formulated international guidelines for NAFLD prevention and treatment.
In terms of epidemiology, the team is the first to clarify the natural history of NAFLD, its pathogenic progression and associated risk factors. In addition, they revealed that NAFLD is an independent risk factor for coronary heart disease, while diabetes is a high-risk factor of NAFLD. Overall, the team has delivered over 190 SCI publications related to NAFLD, and 59 of them are published in journals with an impact factor greater than 10. This superlative work has been acknowledged and included in 14 internationally renowned guidelines for NAFLD. As the pioneer, the team has led clinicians around the globe to formulate “Asia-Pacific Working Party on Non-alcoholic Fatty Liver Disease Guidelines”.