CUHK Advocates Stringent Control of Cardiovascular Risks for Reopening of Narrowed Brain Arteries - A New Paradigm to Prevent Recurrent Stroke (Available in Chinese only)
1. 研究背景
- 中風屬於急性病症,是本港成年人永久致殘的主因
- 中風主要分為兩種類型:一種是由血栓或栓塞所造成的缺血(缺乏血液供應)(ischemic stroke);一種是由出血所造成的(hemorrhagic stroke)
- 整個亞洲區內,誘發缺血性中風的最普遍成因是髗內血管粥樣硬化 (Intracranial Atherosclerotic Disease – ICAD / intracranial stenosis)
- 據以往統計,患者一年內復發率可高至20%,顯示沿用的藥物治療方案效果有欠理想
2. 研究目的
- 透過前瞻性、學術導向的研究,評估症狀性腦動脈粥樣硬化在藥物治療下的演變過程,有助提供科學依據來了解中風復發機制及優化預防策略
3. 研究方法
在2006年至2013年間,招募了50位因高程度(≥70%)腦動脈粥樣硬化狹窄導致(high-grade ICAD stenosis)的中風患者(平均年齡63.4歲)參與研究。
參加者分別於藥物治療開始前及開始後12個月接受3D旋轉血管造影檢查(3-dimentional rotational angiography – 3DRA),以評估腦動脈粥樣硬化演變情況
參加者接受嚴格的藥物治療方案,以控制容易導致心血管疾病的高危因素,見下表:
現行中風患者藥物治療控制指標與更嚴格的標準對比
風險因素 Risk Factors | 現行指標 Current Baseline | 研究倡議之新標準 Suggested Baseline |
|---|---|---|
| 戒煙 | 建議戒煙 | 建議戒煙並積極跟進 |
低密度蛋白膽固醇 (low-density lipoprotein) | <2.6mmol/L | <1.8 mmol/ |
糖化血色素 (glycosylated hemoglobin / HbA1c) | 7.0% | 6.0% |
收縮壓 (systolic blood pressure) | <140mmHg | <130mmHg condition of patients) |
- 另外,我們亦評估了中風復發患者的腦梗塞形態學(infarct topography),並對其進行了微栓子(microemboli)監測
- 對照組為143位腦動脈粥樣硬化狹窄導致的中風患者
(參與了本中心另一項已經發布成果的研究)
4. 研究結果
- 總體而言,動脈粥樣硬化狹窄由79%降至63%(p<0.001)
- 90%參加者的腦血管硬化閉塞沒有加重或出現顯著好轉(詳見下表)
患者動脈粥樣硬化狹窄演變情況 Qualifying Lesions | 人數 (佔總人數比率) Number (%) |
|---|---|
顯著好轉(狹窄程度降低>10%) Remarkably regressed (stenosis reduced >10%)
| 24位 (49%) |
閉塞沒有加重(狹窄程度降低±10%) Remained quiescent (stenosis same or ±10%)
| 21位 (43%) |
加重 (狹窄程度增高>10%) Progressed (stenosis increased >10%) | 4位 (8%) |
- 在危險因素控制力度上,所有患者(包括出現或未出現中風復發,或是狹窄好轉/無加重/加重)均無差別
- 接受藥物治療前糖化血色素越高的患者出現更為明顯的狹窄好轉
- 在一年後的臨牀及血管造影跟進中,發現6位患者出現了中風復發,其中5位的腦梗塞型態為沿著內部或前分水嶺區單一的、或串珠樣病灶(soitary or rosary like acute infarcts along the internal or anterior boarder zones),2位在經顱多普勒超聲(transcrania Doppler ultrasound - TCD)檢查中出現微栓子陽性(microemboic signals)。
- 新藥物治療方案成功令中風復發率由23%降至14%
5. 總結
經12個月的嚴格藥物治療後,大多數的症狀性動脈粥樣硬化狹窄閉塞沒有加重或出現顯著好轉
動脈-動脈栓塞(artery-to-artery thromboembolism)並分水嶺區血管的栓子清除率下降(impaired washout at boarder zones)則為中風復發(stroke recurrence)的常見機制
研究結果已於國際期刊Annals of Neurology 2015年3月號發表,期望此中風藥物治療的新標準將使本港,以至亞洲更多中風患者受益

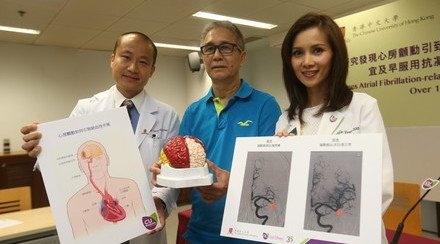
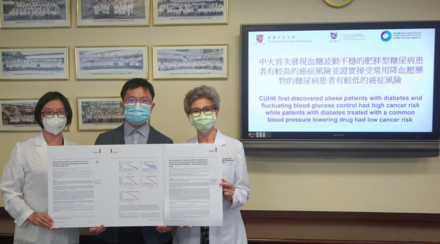
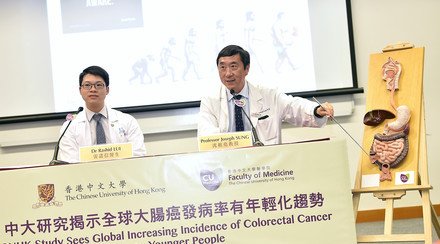
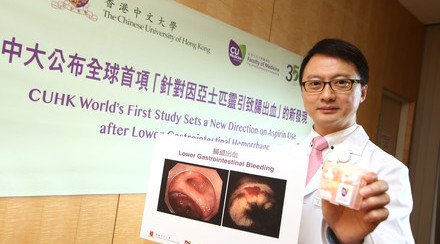
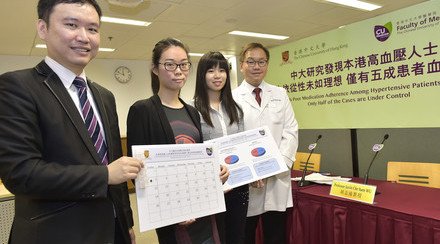
(From left) Dr. Thomas Wai Hong LEUNG, Lee Quo Wei Associate Professor of Neurology, and Dr. Yannie Oi Yan SOO, Clinical Assistant Professor (honorary), from the Department of Medicine and Therapeutics at CUHK advocates a stringent control of cardiovascular risk factor to reopen narrowed brain arteries. By the end of the first year of the study, the high-grade arterial stenosis either remained quiescent or remarkably regressed in over 90% of the participants.

The arterial stenosis of Mr. Lo (middle), who was diagnosed stroke 5 years ago, has diminished from 79% to 58% after a year of aggressive medical approach in controlling risk factors such as blood sugar, blood pressure and lipid levels.