CUHK’s Margaret K.L. Cheung Research Centre for Management of Parkinsonism develops a new tissue imaging technique for studying brain diseases

Researchers from the Margaret K.L. Cheung Research Centre for Management of Parkinsonism at CU Medicine has developed a fast, user-friendly technique to make chemically stabilised antibodies for rapid labelling and imaging of molecules in biological tissues. The novel technique can produce a more comprehensive 3D structural image of the brain which can accelerate the path towards new tools for disease diagnosis and treatment paradigms in the future.
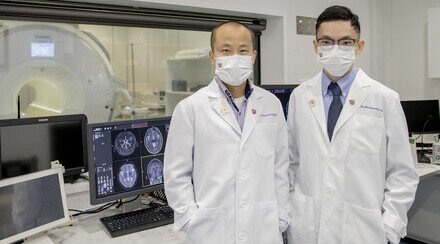
From left: Ms Yumi Tang, Investigator, Margaret K.L. Cheung Research Centre for Management of Parkinsonism and co-first author of the study; Dr Owen Ko, Associate Director of the Research Centre and Professor, Department of Medicine and Therapeutics and School of Biomedical Sciences, CU Medicine; Ms Margaret Cheung; Professor Vincent Mok,Director of the Research Centre; Dr Lai Hei-ming, Principal Investigator of the Research Centre and Assistant Professor, Department of Psychiatry, CU Medicine; and Dr Zachary Lau, Investigator of the Research Centre and co-first author of the study.
With the population ageing globally, neurological conditions such as Parkinson’s disease, Alzheimer’s disease and cerebral small vessel disease impose heavy socioeconomic burdens. To advance diagnostic and treatment methods, it’s crucial to study the pathological processes using animal disease models and human brain tissues. However, currently available techniques for the visualisation of brain structures are limited and costly. To tackle this challenge, the Margaret K.L. Cheung Research Centre for Management of Parkinsonism at The Chinese University of Hong Kong (CUHK)’s Faculty of Medicine (CU Medicine) has developed a fast, user-friendly technique to make chemically stabilised antibodies for rapid labelling and imaging of molecules in biological tissues. The research findings have been selected as the cover story by the latest issue of renowned peer-reviewed journal Nature Methods.
A new technique to visualise the 3D structures of biological tissues
Techniques to visualise the structures of biological tissues are very important for studying the functions of organs such as the brain, both in normal conditions and when suffering from a disease. A technique called immunostaining, which uses antibodies to target biological molecules in tissues, is very powerful and widely used for such purposes. However, antibodies cannot reach deep into the tissues, hindering their application to high-throughput, three-dimensional structural studies. A research team led by Dr Lai Hei-ming, Assistant Professor in CU Medicine’s Department of Psychiatry and Principal Invesitigator of the Margaret K.L. Cheung Research Centre for Management of Parkinsonism; and Dr Owen Ko, Assistant Professor in CU Medicine’s Department of Medicine and Therapeutics and the School of Biomedical Sciences, and Associate Director of the Margaret K.L. Cheung Research Centre for Management of Parkinsonism, invented a 3D immunolabelling strategy named ThICK (thermal immunohistochemistry with optimised kinetics) staining to overcome the limitation.
Dr Lai explained that, “Usually antibodies are sensitive to heat and chemicals called denaturants. When used in immunostaining, these properties limit the choice of temperature and denaturants, since they can destabilise the antibodies and make them lose their functions.”
The team therefore developed a chemical technology that can convert commercially available antibodies, making them much more resistant to heat and denaturants. The heat-stable antibodies, termed SPEARs (synergistically protected polyepoxide-crosslinked Fab-complexed antibody reagents), can be used to achieve immunolabelling of biological molecules deep inside intact tissues by flexibly choosing different incubation temperatures and denaturing chemicals. The use of SPEARs in ThICK staining can help to overcome the limitations of deep 3D immunostaining and optimise the visualisation of brain structures.
SPEARs provide the benefits of a more stable antibody and higher macromolecular diffusivity
SPEARs enable a new approach that is rapid, simple and highly scalable. The study shows that ThICK staining with SPEARs can achieve whole mouse brain immunolabelling within 72 hours; when applied to human brain tissues, it can achieve nearly fourfold deeper penetration with threefold fewer antibodies.
Dr Zachary Lau and Ms Yumi Tang, investigators of the Margaret K.L. Cheung Research Centre for Management of Parkinsonism shared co-first authorship of the research, which contributed to overcoming important technical challenges in making ThICK staining with SPEARs possible. Dr Lau explained that, “ThICK staining achieves whole-organ immunolabelling faster than other state-of-the-art methods, from requiring one to eight weeks for each round of antibody staining to a much shorter time of one to three days.” Ms Tang added, “This new method is compatible with a wide range of commercially available antibodies, and different classes of tissue preservation and clearing methods. It can therefore be readily implemented in most laboratories.”
Dr Ko remarked, “SPEARs are our new weapons. This new technique is especially applicable to the study of neurodegenerative diseases. We hope our work can accelerate the path towards new tools for disease diagnosis and treatment paradigms in the future.”
Dr Lai and Dr Ko are also principal investigators at the Li Ka Shing Institute of Health Science, where their research laboratories are based. This study was also funded by the Croucher Foundation, the National Natural Science Foundation of China, the Innovation and Technology Commission, and the Research Grants Council of Hong Kong.

The research article is selected as the cover story of renowned peer-reviewed journal Nature Methods.
About Margaret K.L. Cheung Research Centre for Management of Parkinsonism
With a generous donation from Ms Margaret Cheung Kam-ling, the Margaret K.L. Cheung Research Centre for Management of Parkinsonism was established in 2019 to conduct transdisciplinary research that unravels disease mechanisms and enables the discovery of therapeutics for preventing or slowing the progression of common diseases that cause parkinsonism.