Dear readers, With the launch of e-newsletter CUHK in Focus, CUHKUPDates has retired and this site will no longer be updated. To stay abreast of the University’s latest news, please go to https://focus.cuhk.edu.hk. Thank you.
Tracking a Silent Killer
Henry Chan did the math of liver cancer for patients and general practitioners

Liver cancer is a silent killer. The disease does not manifest itself until the very late stages–at which point it is often too late to do much for patients. But the disease is surprisingly easy to treat if it is caught early enough.
To that end, CUHK medical professor Henry Chan has developed a scoring system that helps estimate the likelihood of a patient contracting liver cancer in patients who have chronic hepatitis B. He first began identifying patients with a high level of HBV DNA, the virus that causes liver cancer. The accuracy of the score has been improved with the advent of the FibroScan machine, which improves on ultrasound as a way of measuring liver cirrhosis.
Liver stiffness is important as an input because it also reflects the likelihood of liver cirrhosis, and thereby helps identify patients with a high risk of developing hepatocellular carcinoma, the most-common form of liver cancer. Beyond the FibroScan machine analysis, the only other factor necessary to compile the score is a blood test, helping identify the liver-cancer virus and the other inputs.
The scale runs from 0 to 44.5, but it is not linear. A score of 5 is mid-risk, while anything over 20 means the patient is high-risk. A general practitioner should refer patients who score 5 and above to a specialist, Professor Chan says.
A mid-score on the test means a patient has a 5% chance of contracting liver cancer each year, meaning the subject should visit a specialist regularly. Professor Chan first developed the score for patients who haven’t received treatment for liver cancer, and then validated it with patients who are already receiving anti-viral treatment because they have already contracted or appear about to contract liver cancer.
The results have been confirmed not only in his own studies but also independently in other nations, where the system has often been adopted either as is, or in a modified fashion to reflect local conditions.
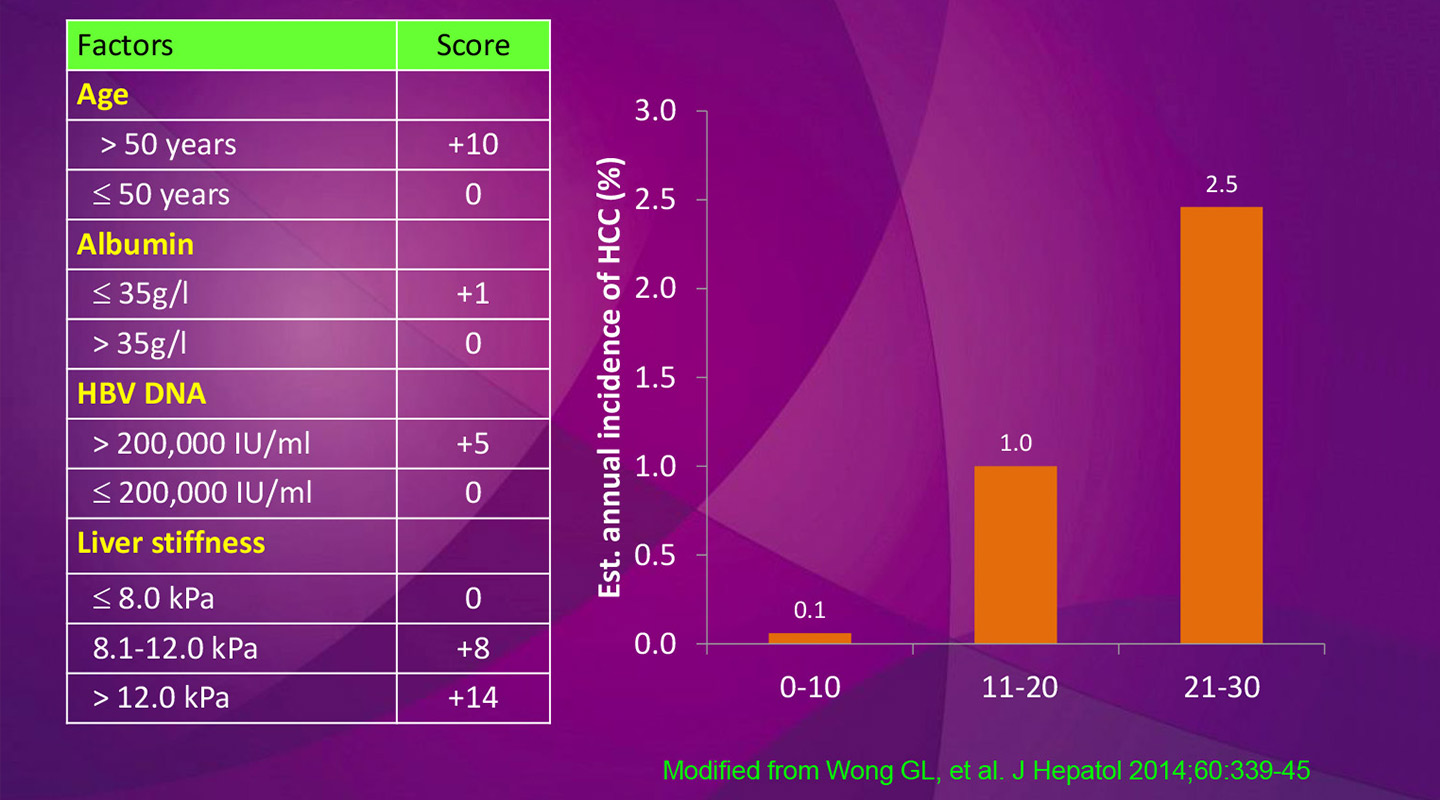
Professor Chan first published his discovery that the HBV DNA virus heightens the risk of contracting liver cancer in the Journal of Clinical Oncology, in 2008. He followed that up with a 2010 paper outlining his scoring system, and a 2014 paper in the Journal of Hepatology studying the importance of liver stiffness in identifying at-risk patients.
The test, known as the CU-HCC model, has the highest score yet recorded on the ‘AUROC’ statistical test: the Area Under Receiver Operating Characteristic Curve. On that scale, a score of 1 means a perfect correlation between screening and identifying liver cancer. A score of 0.5 means the relationship is essentially random.
The CU-HCC model scores 0.85 with Asian patients, who contract hepatitis more often. There is an almost-perfect match of 0.91 with Western patients, who contract liver cancer less frequently, resulting in fewer patients to screen.
The scoring system is particularly useful for family doctors. General practitioners often lack the expertise to determine whether a patient is likely to contract or already has liver cancer. This leaves them in a dilemma. Should they ignore the issue at risk of harming the patient, or should they refer many patients to specialists at public hospitals, overloading the system?
High-risk patients can be slated for stringent testing, such as taking an ultrasound every six months. Low-risk patients can be referred back to their G.P. and simply have a blood test taken periodically as part of routine care.
At the moment, only one-third of the patients in hospital for potential liver cancer fall in the ‘high risk’ camp. Two-thirds are low-risk, out of an already-biased population of people who have already been hospitalized, resulting in an overloading of the public-health system.
The thinning of the herd should make it much more efficient for the liver specialists to hunt down the sick. If they can capture those people early enough, their cancer can be treated.
‘It is very curable,’ Professor Chan says, assuming the cancer is picked up before a tumor grows beyond two centimetres. Even a growth as large as five centimetres can be combatted. Surgery is an option, but so is local ablative therapy. ‘People use many different treatments that we can do without a knife.
The problem is that, to date, scientists have managed to find few ways to combat liver cancer, unlike some other equally deadly forms. ‘If lung cancer is an adult, then liver cancer is an infant,’ Professor Chan says.
Patients do not lose weight. They do not feel pain. Only when the tumor has transformed into the terminal stage does it begin to affect its carrier. And by then it is too late.
Apparently-healthy hepatitis patients therefore also need frequent screening. Doctors in Japan, South Korea and Toronto have all tested Professor Chan’s scoring system and found it effective in identifying and then treating cancer carriers in the early stages of the disease. Singapore is employing a modified form of the test.
Around 9% of the adult population carry the hepatitis B virus in Asia, where it is especially prevalent, particularly among Chinese people.
Hong Kong began vaccinating babies for hep B in 1989. But China only began that process in 1992, and only made the tests free in 2006. So until 10 years ago, the vast majority of the population was unprotected against the disease.
Previously, family doctors had been told to refer patients with a high load of the hep B virus to a specialist. ‘But what is high?’ Professor Chan asks. Family doctors who aren’t familiar with the disease don’t know. And that means they can’t explain the situation to patients either, without scaring them, or letting them go untreated.
‘But if there’s a score, it’s much clearer,’ Professor Chan says. ‘If you can say, "You have a low score, so there’s hardly any chance of you contracting liver cancer. But if you have a mid-score, there’s a 5% chance of you contracting cancer per year, and you have to see a specialist," that is a very easy communication.’
By Alex Frew McMillan
This article was originally published on CUHK Homepage in Jan 2017.