Some COVID-19 patients develop various persistent symptoms weeks and months after completely recovering from the infection. Investigators from the Department of Ophthalmology and Visual Sciences of The Chinese University of Hong Kong’s (CUHK) Faculty of Medicine (CU Medicine) have found that 1 in 5 post-COVID patients have at least one recent-onset symptom related to the dry eye disease (DED), such as blurring, itch and pain or burning sensation. In addition, the study showed that the risk of DED is linked to the severity of COVID infection. The findings have recently been published in the international journal Clinical and Experimental Ophthalmology (the official journal of The Royal Australian and New Zealand College of Ophthalmologists).
Symptoms of DED include grittiness, pain, blurred vision, and more
Affecting tens of millions of individuals globally, DED is a major reason for patients seeking eye care. In Hong Kong, the estimated prevalence is 30%. DED is characterized by an unstable and a more concentrated (termed “hyperosmolar”) tear film, leading to increased inflammation and damage to ocular surface structures and nerves. Symptoms of DED include grittiness, pain or soreness, burning, watering, light sensitivity, and blurred vision. DED carries significant socioeconomic implications, including medical costs and disruption of work in prime life.
Professor Clement CY THAM, Chairman and S.H. Ho Professor of Ophthalmology and Visual Sciences, Department of Ophthalmology and Visual Sciences, CU Medicine said, “DED can significantly impair daily social and physical functioning, such as reading, uses of digital devices and driving. The increased time and cost spent on treatment and the avoidance of specific environments in the workplace that aggravate dry eye symptoms decrease workplace productivity.”
Professor Calvin CP PANG, S.H. Ho Research Professor of Visual Sciences, CU Medicine has been studying the ocular effects of COVID on adults and children. “COVID can have direct clinical effects on people’s eyes. It also affects people’s vision indirectly through disruptions of normal working and living activities.”
Post-COVID patients have a greater risk of dry-eye-related ocular surface manifestations
The CUHK research team evaluated 228 post-COVID patients, who were diagnosed between February and December 2020, one to three months after their diagnoses, and 109 healthy age-matched participants. All participants received comprehensive eye examinations. Participants with any pre-existing ocular surface conditions, previous history of refractive surgery, ophthalmic surgery, ocular trauma, contact lens used within the past three months, or using any eye medication were excluded.
During the study, all participants underwent comprehensive eye examinations including evaluation for meibomian gland dysfunction, the most common cause of DED, and corneal fluorescein staining, an indicator of DED severity. It was found that post-COVID patients had a higher prevalence of dry-eye-related ocular surface manifestation than healthy individuals. (Please refer to table 1 in the appendix for full data)
Among post-COVID patients who received any form of supplementary oxygen during hospitalization, their tear break-up time (an indicator for tear evaporation) was 1.6 seconds shorter, when compared to those not requiring oxygen during hospitalization, one of the reasons being the gas flow from oxygen delivery may increase the evaporation of the tear film.
Dr. Kelvin HN WAN, the lead author of the study and Assistant Professor, Department of Ophthalmology and Visual Sciences of CU Medicine said, “Besides, we found that every 1-point reduction in Ct-value (inversely correlated with the viral load) from the respiratory specimen collected at hospital admission increased the risk of having any dry-eye-related ocular surface symptoms during the first month after recovery by 10%. This finding suggests the risk of tear film instability after recovery from COVID is associated with the severity of the acute infection.”
The post-COVID patients were enquired about their dry-eye-related ocular surface symptoms after COVID-19 diagnosis using a questionnaire at the time of ophthalmic assessment after discharge. Over 20% of post-COVID patients (21.5%) had at least one of these new symptoms, most commonly blurred vision (9%), itch (6.1%), pain or burning sensation (4.8%), tearing or discharge (3.9%), and redness (3.1%). (Please refer to table 2 in the appendix for full data)
Dr. Kelvin KL CHONG, principal investigator of the study and Associate Professor, Department of Ophthalmology and Visual Sciences, CU Medicine said, “The outcome of our study is one additional strong reason why each one of us should complete our COVID-19 vaccination regime as soon as possible. A completed vaccination regime is currently the most important and effective measure one can take to significantly ‘raise the Ct value’, that is to lower the disease severity if infected, and decrease the chance of developing severe COVID-19 requiring supplementary oxygen. Vaccination remains the most effective measure in preventing post-COVID-19 eye symptoms and all other longer-term sequelae.”
The study was supported by Health and Medical Research Fund, Hong Kong SAR, project number COVID190106.
Appendix
Table 1: Comparison of the dry-eye-related ocular surface manifestation between post-COVID patients and healthy individuals:
| Post-COVID patients | Healthy individuals | |
| Meibomian gland dysfunction staging# | 1.14±0.67** | 0.92±0.68 |
| Proportion of eyes with any positive corneal fluorescein staining | 48.9%* | 38.6% |
| Corneal fluorescein staining score# | 0.60±0.69* | 0.49±0.68 |
| Statistical significance *p<0.05, **p<0.005 Remarks: # Graded on a 4-point scale (0=absent, 1=mild, 2=moderate, 3=severe) |
||
Table 2: Summary of the prevalence of recent-onset dry eye symptoms among post-COVID patients:
| Dry eye symptoms | Percentages of post-COVID patients presenting related symptoms |
| Blurring | 9.2% |
| Itch | 6.1% |
| Pain or burning sensation | 4.8% |
| Tearing or discharge | 3.9% |
| Redness | 3.1% |
| Grittiness | 2.2% |
| Light-sensitivity | 1.8% |
| Lid swelling | 1.3% |
| One or more than one related symptoms | 21.5% |
中大醫學院研究顯示新冠康復者有較高機會出現乾眼症
部份新型冠狀病毒病(新冠)患者在康復後數周甚至數月,仍然會持續出現一些身體問題或後遺症。香港中文大學(中大)醫學院眼科及視覺科學學系的研究團隊發現,每五名新冠康復者中就有一人感染後出現最少一種與乾眼症相關的症狀,例如視力模糊、眼睛瘙癢、疼痛或燒灼感等;患者的新冠病情愈嚴重,出現乾眼症的風險愈高。研究結果已在國際期刊Clinical and Experimental Ophthalmology(澳洲及新西蘭皇家眼科醫學院的官方期刊)中發表。
乾眼症的症狀包括眼澀、疼痛、視力模糊等
乾眼症影響全球數以千萬計人口,亦是病人尋求眼科醫生診症的主因之一。香港的患病率估計達30%。乾眼症是由於淚膜不穩定及淚液的滲透壓增加(稱為「高滲性」),導致眼球表面出現炎症並對眼睛表面結構和及眼表神經造成損害。乾眼症狀包括眼澀、疼痛或酸痛、灼熱感、流淚、畏光和視力模糊。乾眼症對社會及經濟層面亦帶來顯著負擔,包括增加醫療費用的開支和影響患者青壯年時期的工作效率。
中大醫學院眼科及視覺科學學系系主任兼何善衡眼科及視覺科學講座教授譚智勇教授表示:「乾眼症會顯著影響個人的日常生活和社交功能,例如閱讀、使用電子產品和駕駛。患者需要花費大量時間及金錢進行治療,亦要避免工作場所中會加劇乾眼症狀的環境,這大大降低他們的工作效率及生產力。」
中大醫學院何善衡視覺科學研究講座教授彭智培教授一直研究新冠病毒對成年人和兒童眼部的影響:「新冠病毒不但可以直接引致眼疾,也會通過影響正常的學習和生活習慣,間接損害我們的視力。」
新冠康復者有較高風險出現乾眼症及相關的眼表症狀
中大研究團隊為確診1至3個月內的228名新冠確診者(確診於2020年2月至2020年12月)和109名健康人士進行了全面的眼科評估及檢查。所有參加者均經過嚴謹篩選,以確保他們在參加研究前沒有患任何眼表疾病或眼外傷、未曾接受矯視手術或眼科手術、未曾使用任何眼科藥物或過去 3 個月內未曾配戴過隱形眼鏡。
研究人員為參加者進行全面的眼科評估及檢查包括「瞼板腺功能障礙檢查」(瞼板腺功能障礙為乾眼症最常見原因)和「角膜螢光素染色試驗」(乾眼症嚴重程度的指標)。綜合各項數據發現新冠康復者出現乾眼症狀的指數略高於一般健康人士(詳細數據可參閱附件表一)。
研究人員亦發現,住院期間需要接受任何形式氧氣補充的新冠康復者,他們的淚液破裂時間(淚液蒸發率的指標)比不需要接受氧氣補充治療的患者縮短了原因之一是相信與接受氧氣補充治療時,氣體在鼻腔的流動加速了淚液蒸發有關。
是次研究文章的首席作者及中大醫學院眼科及視覺科學學系助理教授尹浩柟醫生表示:「我們發現新冠患者入院時採集的呼吸道樣本CT 值每低1個值(CT值愈低代表病毒量愈高),在康復後的第一個月內出現任何乾眼症相關眼表症狀的風險就會增加約10%。即代表新冠病情愈嚴重,其後患上乾眼症狀的風險亦會相應增加。」
除了接受眼科檢查,出院後的新冠康復者同時進行了乾眼相關眼表症狀的問卷評估。結果顯示,超過兩成新冠康復者(21.5%)在新冠感染後,出現至少一種新症狀,最常見分別的是視力模糊(9%)、瘙癢(6.1%)、疼痛或燒灼感(4.8%)、流淚或分泌物(3.9%)、眼紅(3.1%)等。(詳細數據可參閱附件表二)
研究的首席研究員及中大醫學院眼科及視覺科學學系副教授莊金隆醫生表示:「我們的研究結果是一個有力的理由支持大家盡快完成新冠疫苗接種。疫苗接種是目前最重要和最有效的措施,可以顯著可以顯著減少感染後的病毒量 (提高Ct值) 、減少患上重症、並需要氧氣補充治療的機會。接種疫苗也是預防新冠後眼部症狀和所有其他後遺症的最有效措施。」
本研究由香港特別行政區食物及衞生局醫療衞生研究基金資助,參考編號 COVID190106。
附件
表一:新冠康復者與健康人士之間的眼表症狀比較:
| 新冠康復者 | 健康人士 | |
| 瞼板腺功能障礙分數# | 1.14±0.67** | 0.92±0.68 |
| 出現任何角膜螢光素染色試驗陽性的比例 | 48.9%* | 38.6% |
| 角膜螢光素染色試驗分數# | 0.60±0.69* | 0.49±0.68 |
| 註:差異有統計學意義 *p<0.05, **p<0.005 #以4分制進行評分(0 = 不存在,1 = 輕度,2 = 中度,3 = 嚴重) |
||
表二:新冠康復者感染後出現乾眼相關眼表症狀的問卷評估:
| 眼乾相關眼表症狀 | 曾經出現相關症狀的康復者比率 |
| 視力模糊 | 9.2% |
| 瘙癢 | 6.1% |
| 疼痛或燒灼感 | 4.8% |
| 流淚或分泌物 | 3.9% |
| 眼紅 | 3.1% |
| 眼澀 | 2.2% |
| 畏光 | 1.8% |
| 眼瞼腫脹 | 1.3% |
| 出現任何一種或多於一種症狀 | 21.5% |
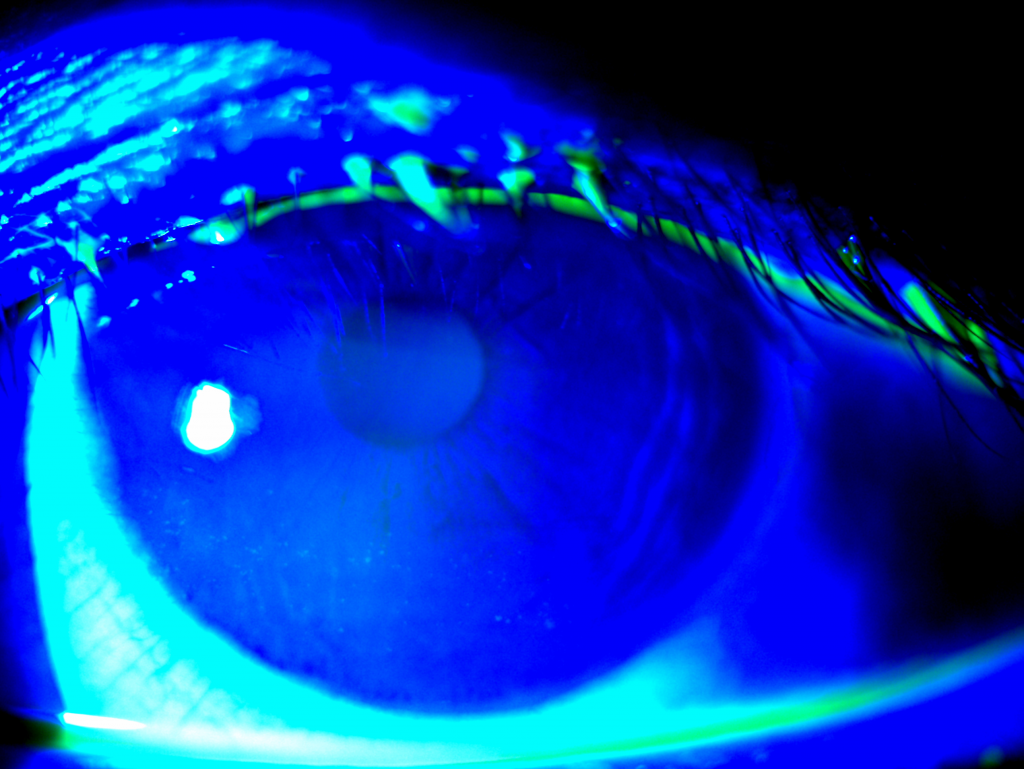
乾眼症患者的角膜表皮出現輕度破損(俗稱「角膜爆拆 」)

輕度瞼板腺功能障礙的乾眼症患者。


 Creative Commons Attribution-NonCommercial
Creative Commons Attribution-NonCommercial