|
|
|
Chapter 1
Understanding common bowel changes in older adults Case study – Story of Ms. Lau 10 Myths and misconceptions of bowel habit What should the stool look like? Case study – Common bowel problems among older adults in HK - End of Chapter 1- Reference Canadian Society of Intestinal Research. (2020). Aging Digestive Tract. Retrieved from https://badgut.org/wp-content/uploads/GIS-PIH-AN-2020-06.pdf Centre for Health Protection. (2014). Constipation - Find the Way Out. Retrieved from https://www.chp.gov.hk/files/pdf/ncd_watch_mar2014.pdf Centre for Health Protection. (2018). Know more about fat. Retrieved from Continence Foundation of Australia. (2020). Bristol stool chart. Retrieved from https://www.continence.org.au/bristol-stool-chart Lewis, S.J., & Heaton, K.W. (1997). Stool form scale as a useful guide to intestinal transit time. Scandinavian Journal of Gastroenterology, 32(9), 920-4. Schuster, B.G., Kosar, L., & Kamrul, R. (2015). Constipation in older adults: Student Health Service. (2018). Diet & nutrition. Retrieved from Walter, S.A., Kjellström, L., Nyhlin, H., Talley, N.J., & Agréus, L. (2010). Assessment of normal bowel habits in the general adult population: the Popcol study. Scandinavian Journal of Gastroenterology, 45(5), 556-66. 衛生防護中心(2014年3月)。〈為便秘找出路〉。取自https://www.chp.gov.hk/files/pdf/ncd_watch_mar2014_chin.pdf Chapter 2
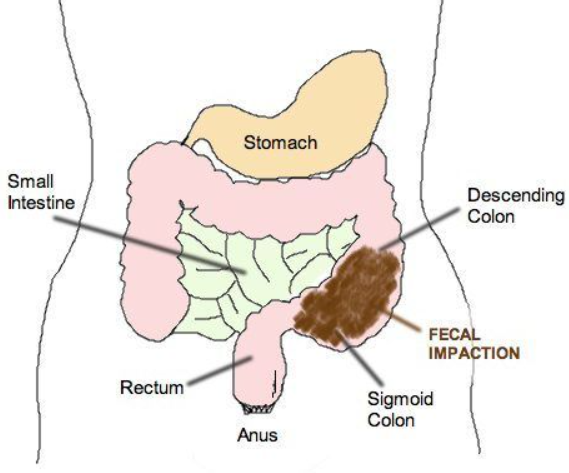
Constipation in older adults What is constipation? Constipation among older adults What is faecal impaction?
(You may refer to Video 1 – Case Study - Story of Ms. Lau. Jane has bought antidiarrheal medication for Ms. Lau but her condition was even getting worse.)
(Image source from: https://www.pinterest.com/pin/182536591131752406/)
- commonly found in older adults with neuropsychiatric disorders (e.g. Alzheimer disease, Parkinson disease, and severe stroke)
The incidence of fecal impaction increases with age and dramatically impairs the quality of life in older adults.
A study indicated that constipation is particularly relevant occurring in up to 66% among PD patients, thus showing a higher prevalence than within the general population (Pedrosa Carrasco, Timmermann & Pedrosa, 2018).
Untreated fecal impaction can result in serious health complications:
Age, acuteness of symptoms, and medication history is important to exclude various causes of constipation.
Complete blood count, serum calcium, glucose levels, and thyroid function tests are generally adequate to screen for underlying metabolic or other organic pathology
It is important in the primary care setting. A rectal exam can reveal rectal tumours, haemorrhoids, impacted faeces, anal sphincter tone, presence of mucus, stool colour and palpation of abdominal mass.
It is a simple, non-invasive investigation that may show faecal impaction. Advanced diagnostic procedures, such as barium enema, defaecography, colonic transit studies, magnetic resonance imaging, manometry, and balloon expulsion test should be reserved for patients with suspected slow transit constipation and defaecatory disorder in the specialist care setting.
Fecal impaction can be treated with medication and may require a procedural intervention for particularly resistant situations. 1. Oral laxatives: - The first line of treatment involves the use of laxatives to soften the hardened stool so that it can be passed. 2. Suppositories: - Sometimes a laxative is used as a suppository, meaning that it is taken in a form that is inserted into the rectum, rather than taken by mouth. It works more quickly than an oral laxative and is a preferred method if the impaction is particularly distal (low down) in the colon. 3. Enema: - An enema is the introduction of liquid, most often Bisacodyl, mineral oil or saline solution, through the anus and into the large intestine. The goal is to loosen stuck stool and encourage a bowel movement. Enema is generally recommended when first-line treatments have not worked. 4. Water irrigation: - It is a medical procedure that performed by health care professionals. A tube is inserted through patient’s anus and then injects water into the rectum to loosen the stool, allowing to have a bowel movement. 5. Manual evacuation: - Used in severe cases. - Areas of faecal impaction will be located by feeling the outside of your abdomen, stool is emptied by gently inserting a finger into the rectum and removing it. Hemorrhoids Management of Hemorrhoids among older adults Medical treatment of hemorrhoids
Medical treatment will depend on the symptoms of hemorrhoids. They usually prescribe topical creams and ointments or suppositories as a first line treatment. These medications contain steroids which reduces inflammation and relieves pain. Some of them also have anesthetic effects to relieve the discomfort. It should be noted that medication can only relieve the symptoms, but not eliminate the hemorrhoids. If the hemorrhoids are severe, they can be removed by surgery. However, people usually mistakenly think that removing the hemorrhoids surgically can cure the problem. Since hemorrhoids are caused by varicose veins in the rectum, even if the hemorrhoids are removed, if the poor lifestyles persist, the remaining blood vessels in the rectum will also be persistently compressed, and hemorrhoids may still recur. Therefore, it is very important to maintain healthy lifestyles, such as eating enough vegetables and fruits, getting enough water, doing more exercise, increasing activity level, reducing abdominal pressure, and maintaining good bowel habits. - End of Chapter 2- Reference Alzheimer Scotland. (2011). Constipation & faecal impaction. Retrieved from American College of Gastroenterology. (2012). Chronic constipation linked to increased risk of colorectal cancer. Retrieved from https://www.sciencedaily.com/releases/2012/10/121022081228.htm Best Practice Advocacy Centre New Zealand. (2019). Managing constipation in older people. Retrieved from https://bpac.org.nz/2019/constipation.aspx Centre for Health Protection. (2010a). Behavioural Risk Factor Survey. Retrieved from Centre for Health Protection. (2010b). Men's health line – Haemorrhoid. Retrieved from https://www.chp.gov.hk/en/static/80041.html Centre for Health Protection. (2020). Men's health line – Constipation. Retrieved from https://www.chp.gov.hk/en/static/80034.html Continence Foundation of Australia. (2015). Parkinson's and constipation. Retrieved from https://www.continence.org.nz/pages/Parkinsons-and-constipation/129/ Dumic, I., Nordin, T., Jecmenica, M., Lalosevic, M.S., Milosavljevic, T., & Milovanovic, T. (2019). Gastrointestinal Tract Disorders in Older Age. Canadian Journal of Gastroenterology and Hepatology, 2019, 6757524. https://doi.org/10.1155/2019/6757524 Elderly Health Service. (2020). Constipation. Retrieved from Harvard Health Publishing, Harvard Medical School. (2008). Harvard women's health watch: What to do about hemorrhoids. Retrieved from https://www.health.harvard.edu/mens-health/what-to-do-about-hemorrhoids Harvard Health Publishing, Harvard Medical School. (2019). Hemorrhoids. Retrieved from https://www.health.harvard.edu/a_to_z/hemorrhoids-a-to-z Nebhinani, N., & Suthar, N. (2017). Constipation in elderly patients with psychiatric disorders. Journal of Geriatric Mental Health, 4(1),11. Obokhare, I. (2012). Fecal Impaction: A Cause for Concern? Clinics in Colon and Rectal Surgery, 25(1), 53–8. https://doi.org/10.1055/s-0032-1301760 Parkinson's Disease Foundation. (2016). Understanding Parkinson's Constipation and PD. Retrieved from https://www.parkinson.org/sites/default/files/attachments/constipation_16.pdf Pedrosa Carrasco, A.J., Timmermann, L., & Pedrosa, D.J. (2018). Management of constipation in patients with Parkinson's disease. NPJ Parkinson's Disease, 4, 6. Souza, A. (2007). Ageing and the gut. Postgraduate Medical Journal, 83(975), 44–53. The University of Hong Kong. (2019). Newspaper columns. Retrieved from Wu, J. C. Y., Chan, A. O. O., Cheung, T. K., Kwan, A. C. P., Leung, V. K. S., Sze, W. C., & Tan, V. P. Y. (2019). Consensus statements on diagnosis and management of chronic idiopathic constipation in adults in Hong Kong. Hong Kong Medical Journal, 25(2), 142-8. https://doi.org/10.12809/hkmj187692 香港中文大學那打素護理學院轄下那打素護理實務研究中心。〈機能性便秘之實證護理〉。 2021年1月28日,取自http://www.cuhk.edu.hk/med/nur/nnpru/doc/BowelCareBookletFinal.pdf Chapter 3
Assessment of Constipation Introduction In your daily practice, did you know any older adults who complain of constipation problem? If you want to help, you must know how to assess the problem in order to provide appropriate action. Do you have any idea of how to assess this problem? Let’s discuss about this topic! Assessment of Constipation: • History taking • Red flags • Clinical assessment • Further Investigations History Taking History Taking • A comprehensive history taking help to understand the patient’s condition. If patient has communication problem and unable to provide medical history, caregiver is important resource to collect information. • Medical history • Any past medical history and present complaint? • Any medication in use that may induce constipation? • Any presence of other gastrointestinal symptoms e.g. abdominal pain, bloating, and vomiting? • Investigate the stool form and defaecation pattern such as the time, frequency, amount and consistency of stools. • Any signs of Red flags? • Stool diary Stool Diary Stool Diary • Help to understand the history and current situation of constipation. • Investigate the stool form and defaecation pattern • Ask patient to record the frequency, amount, type and any abnormality of defaecation. Use Bristol stool scale to describe the type of stools. Example of Stool Diary
For details of Bristol stool form scale, please refer to Chapter 1.3. Red Flags Rule out the Red Flags that indicate something more serious, such as colon cancer. Red Flags Alert: • Recent onset of chronic constipation associated with: • Unintentional weight loss • Aneaemia • Abdominal pain • Blood per rectum or presence of faecal occult blood • Unexplained change in bowel habit, involving stool frequency or consistency • Failure to alleviate constipation despite compliance with adequate lifestyle modification • Chronic constipation necessitating use of high doses of laxatives • Recent-onset faecal incontinence Consult family doctor or gastroenterologist if identified any sign of Red Flat. Clinical Assessment Clinical Assessment • Roma IV Criteria • Abdominal examination • Digital rectal examination • Proctoscopy examination • Laboratory investigations • Blood testing including: Complete blood count, Renal function, Electrolytes, Calcium, Glucose, Thyroid function • Faecal occult blood Rome IV Diagnostic Criteria for Constipation Symptoms started six months before diagnosis, and during the last three months, two or more of the following symptoms occurred: (i) Straining in more than 25% of defecations. (ii) Lumpy or hard stools (Bristol stool form scale type 1 or 2) in more than 25% of defecations. (iii) Sensation of incomplete evacuation in more than one-fourth (25%) of defecations. (iv) Sensation of anorectal obstruction/blockage in more than one-fourth (25%) of defecations. (v) Manual maneuvers to facilitate in more than one-fourth (25%) of defecations. (vi) Fewer than three spontaneous bowel movements per week. Further Investigations Referral to gastroenterologist for further investigation such as: • Colonoscopy • Sophisticated investigations • Balloon expulsion test • Colonic transit study • Anorectal manometry • Defaecography - End of Chapter 3- Reference Aziz, I., Whitehead, W. E., Palsson, O. S., Törnblom, H., Simrén, M. (2020) An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation, Expert Review of Gastroenterology & Hepatology, 14(1), 39-46. https://doi.org/10.1080/17474124.2020.1708718 Lacy, B. E., Mearin, F., Chang, L., Chey, W. D., Lembo, A. J., Simren, M., Spiller, R. (2016). Bowel Disorders. Gastroenterology (New York, N.Y. 1943), 150 (6), p.1393-1407.e5. doi: 10.1053/j.gastro.2016.02.031. Sobrado, C. W., Neto, I. J., Pinto, R. A., Sobrado, L. F., Nahas, S. C., Cecconello, I. (2018). Diagnosis and treatment of constipation: a clinical update based on the Rome IV criteria. Journal of Coloproctology, 38, 137-44. https://doi.org/10.1016/j.jcol.2018.02.003 Tong, P. C. (2017). Constipation and Faecal Incontinence. In Kong, T. K. (Ed.), The Hong Kong Geriatrics Society: Curriculum in geriatric medicine (2nd ed.) (pp.201-209). Hong Kong: Hong Kong Academy of Medicine Press. Wu, J. C. Y., Chan, A. O. O., Cheung, T. K., Kwan, A. C. P., Leung, V. K. S., Sze, W. C., & Tan, V. P. Y. (2019). Consensus statements on diagnosis and management of chronic idiopathic constipation in adults in Hong Kong. Hong Kong Medical Journal, 25(2), 142-148. https://doi.org/10.12809/hkmj187692 Zheng, S., Yao, J. (2018). Chinese Geriatric Society, Editorial Board of Chinese Journal of Geriatrics. Expert consensus on the assessment and treatment of chronic constipation in the elderly. Aging Medicine (Milton), 1(1), 8-17. doi: 10.1002/agm2.12013. PMID: 31942474; PMCID: PMC6880707. Chapter 4
Lifestyle modification to prevent constipation Case study - Lifestyles of Ms. Lau High fiber dietary advice What is dietary fibre?
Insoluble and soluble fibre High fibre diet of preventing constipation How to get adequate dietary fibre in our daily menu? Tips to achieve adequate fibre intake
Learn about the fibre content of different kinds of food - Tips to achieve adequate fibre intake 1. Choose wholegrains over refined grains
Fibre content of some common grains and grain products 1 bowl=250ml; Source: USDA. FoodData Central 2019. fdc.nal.usda.gov. 2. Eat a variety of vegetables and fruits
Eat a variety of vegetables and fruits - Vegetables
Fibre content of some common vegetables 1 bowl=250ml; Source: USDA. FoodData Central 2019. fdc.nal.usda.gov. Eat a variety of vegetables and fruits - Fruits
Fibre content of some common fruits 1 bowl=250ml; Source: USDA. FoodData Central 2019. fdc.nal.usda.gov. Eat a variety of vegetables and fruits (2)
3. Include legumes and beans in daily cooking
Fibre content of some common legumes and beans 1 bowl=250ml; Source: USDA. FoodData Central 2019. fdc.nal.usda.gov. 4. Include nuts and seeds in diet
Fibre content of some common nuts and seeds 1 bowl =250ml; Source: USDA. FoodData Central 2019. fdc.nal.usda.gov. 5. Choose high fibre foods as snack
6. Drink enough water
7. Increase fibre gradually
Sample menu with around 25 grams of fibre Can you modify this diet to one with a higher fibre intake?
Hints
- aim for at least 50% of daily grain as wholegrains
- at least 3 serves of vegetables and 2-3 serves of fruits
A modified diet with high fibre High fibre diet recipe Gut microbiome Gut microbiome Regular exercise Recommended exercises to prevent constipation by physiotherapist Pelvic Floor Muscle Stimulation In daily practice, using dry cell driven electrical stimulator to stimulate pelvic floor muscle cam improve the strength and endurance. The electrical pads placement is as shown in the following picture.
(Image source from: https://ars.els-cdn.com/content/image/1-s2.0-S0022346818303804-gr1.jpg) When the electrical stimulator is turned on, electric current would be delivered to the pelvic floor muscle via the electrical pads. When the current intensity is strong enough, the pelvic floor muscles will contract. During current is coming, the subject should voluntarily contract the urethra sphincter muscles and the anal sphincter muscle simultaneously. The former muscle will help to hold the urine from leaking out and the latter will help the bowel empting action respectively. Chinese medicine Constipation – perspectives from Chinese medicine Constipation is a disease of spleen and stomach within the scope of internal medicine of traditional Chinese medicine (TCM). It generally means a decrease of defecation frequency, a difficulty in defecation, straining or a prolongation of defecation time. In terms of modern medicine, constipation is generally classified into organic or functional type. An organic constipation is mainly caused by a substantial disease in organs such as digestive tract disease and endocrine system disease; if the above definite cause is not confirmed for constipation, a functional constipation may be considered. As early as the Warring States Period, constipation was recognized in TCM; its cause was considered as related to coldness of spleen and stomach or heat in intestine. In the late Eastern Han Dynasty, constipation was understood more comprehensively by Zhang Zhongjing (a famous TCM doctor); it was classified into a syndrome of cold, heat, deficiency and excess. Based on such classification, TCM prescription was created for constipation treatment respectively: Chengqi Decoction (bitter flavor, cold nature and purgation effect); Maziren Pills (Yin nourishing and moistened catharsis); and Houpu Sanwu Decoction (Qi-flow regulation and catharsis). Subsequent TCM masters were deeply enlightened by his prospective advocacy. His prescriptions for constipation treatment have been popular until now; they are still common prescriptions for clinical treatment of constipation. For ordinary people, it is normal to defecate once or twice a day. When defecation is made once every not less than 3 days or when defecation frequency is normal but the stool is hard to cause a difficult or incomplete defecation, constipation can be considered. As shown by a foreign statistical investigation, 70% of older adults of >65 years old were vexed at difficult defecation. Compared with young people, older adults are more prone to suffer from constipation, mainly due to a decrease in bowel movement caused by the degeneration of neuromuscular system or other chronic diseases such as diabetes or diseases of nervous system. In addition, due to the degeneration of nervous system in rectum, the activity of anal sphincter and the sensitivity of receptors in rectal wall, an obstructive constipation is caused at rectal outlet. Under general conditions, the severity of constipation will tend to increase with age. In many older adults, due to the retained stool, some discomforts occur such as abdominal distension, abdominal pain and poor appetite, which greatly reduce the quality of their life. Meanwhile, the difficult defecation is closely related to colorectal cancer; thus the risk for colorectal cancer is increased in older adults with constipation. In addition, at a forced defecation, abdominal pressure is increased to change the blood flow in coronary artery and cerebral blood vessel, which have an opportunity to induce serious outcome such as cardiovascular/cerebrovascular accident. Therefore, the constipation in older adults should undoubtedly be closely concerned and solved. Etiology and pathogenesis of TCM for constipation with recommendations on tea and soup Relief of constipation through acupoint pressing Constipation – perspectives from Chinese medicine 1. Properly replenish the water About 1500 mL water is drunk at a fixed time point of every day. For example: At the getup of every day, one cup of warm boiled water is drunk; then an appropriate amount of water is drunk every 2 hours. Through such water replenishing, the necessary moisture can be effectively absorbed by somatic cell so as to prevent the occurrence of constipation. 2. Take more vegetables and foods of high fiber Older adults are suggested to take more vegetables of fiber, such as celery, mustard and cabbage. However, with an insufficient or loose tooth, older adults are more difficult to make a chewing. Therefore, a soup made from high-fiber vegetables is suggested for older adults, such as borscht soup and long-stewed watercress soup. The vegetables cooked to soft state are taken together with soup. Some fruits such as banana or papaya can be taken by older adults to facilitate the defecation. For the people with diabetes, the ground powder of walnut meat, apricot kernel, edestan and sesame can be added to make a pasty diet. 3. Properly avoid a certain food A fried, roasted, greasy or spicy food should be avoided as far as possible, so as to reduce the heat accumulation in gastrointestinal tract. 4. Keep an ease mind, and take appropriate exercise 5. Without prior suggestion of doctor, do not misuse laxatives or folk prescriptions. 6. For older adults with hypertension, avoid a forced defecation so as to prevent the occurrence of cardiovascular/cerebrovascular accident. 7. If the problem of constipation in older adults is not yet solved despite diet therapy, massage or exercise, please turn to medical care personnel. Manual abdominal massage Bowel habit Common laxatives for constipation Common laxatives for constipation Newer pharmacological therapies • Prosecretory agents and Prokinetic agents • Prosecretory agents is the only registered for use in Hong Kong • Used as second-line pharmacological management Type: • Prosecretory agents: Linzess®(Linaclotide) Action: • Promote gut motility and increase intestinal secretion. Side effect: • Diarrhea • Stomach pain • Bloating and flatulence Form: • Tablet Caution: • Monitor renal function for patients who are at risk of dehydration and renal dysfunction. How to use an anal suppository? 1. Wash your hands. 2. Put on disposable gloves if needed. 3. Remove the suppository from the wrapping. 4. Most people find it helps to insert the suppository if it is moistened with a little tap water first. 5. Patient in lateral position and bend the upper leg towards to the chest, lower leg bend slightly.
(Image source from: Hong Kong Emergency Nurses Association) 6. Using a finger, gently push the suppository into your rectum about 3cm depth. 7. Remain still for 10 minutes to help hold the suppository in place. 8. It will start to work in about 15-30 minutes. 9. Remove your gloves. 10. Wash your hands. - End of Chapter 4- Reference AJ Physio. (2018). Good Bowel Habits. Retrieved from https://www.ajphysio.com.au/good-bowel-habits/ Better Health Channel. (2014). Fibre in food. Retrieved from https://www.betterhealth.vic.gov.au/health/healthyliving/fibre-in-food Bharucha, A. E., & Wald, A. (2019). Chronic Constipation. Mayo Clinic proceedings, 94(11), 2340–2357. https://doi.org/10.1016/j.mayocp.2019.01.031 Chinese Nutrition Society. (2013). Dietary reference intakes for Chinese. Retrieved from http://en.cnsoc.org/DRIs/ Dimidi, E. et al. (2014). The effect of probiotics on functional constipation in adults: a systematic review and meta-analysis of randomized controlled trials. The American Journal of Clinical Nutrition, 100(4), 1075-84. Dong, T.S., & Gupta, A. (2019). Influence of early life, diet, and the environment on the microbiome. Clinical Gastroenterology and Hepatology, 17(2), 231-42. Drug Office, Department of Health. (2021). Laxatives and antidiarrheals. Retrieved from https://www.drugoffice.gov.hk/eps/do/en/consumer/news_informations/dm_37.html#a Fernández-Bañares F. (2006). Nutritional care of the patient with constipation. Best Practice & Research Clinical Gastroenterology, 20, 575-87. Gandell, D., Straus, S. E., Bundookwala, M., Tsui, V., & Alibhai, S. M. (2013). Treatment of constipation in older people. Canadian Medical Association journal, 185(8), 663–70. https://doi.org/10.1503/cmaj.120819 Gibson, G.R. et al. (2017). Expert consensus document: The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of prebiotics. Nature Reviews Gastroenterology & Hepatology, 14, 491-502. Healthy WA, Department of Health. (n.d.). Bowel health. Retrieved January 21, 2021, from https://healthywa.wa.gov.au/Articles/A_E/Bowel-health Hill, C. et al. (2017). The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nature Reviews Gastroenterology & Hepatology, 11, 506–14. Lagro-Janssen, T.L., Debruyne, F.M., Smits, A.J. & Weel, C. (1991). Controlled trial of pelvic floor exercises in the treatment of urinary stress incontinence in general practice. British Journal of General Practice, 41(352), 445-9. Martínez-Martínez, M.I., Calabuig-Tolsá, R., & Cauli, O. (2017). The effect of probiotics as a treatment for constipation in elderly people: A systematic review. Archives of Gerontology and Geriatrics, 71, 142-9. Monash University. (2016). Dietary fibre series-resistant starch. Retrieved from https://www.monashfodmap.com/blog/dietary-fibre-series-resistant-starch/ Monash University. (2020). Prebiotic diet – FAQs. Retrieved from https://www.monash.edu/medicine/ccs/gastroenterology/prebiotic/faq University of Michigan Health System. (2011). Healthy Bowel Habits. Retrieved from https://medicine.umich.edu/sites/default/files/content/downloads/healthy-bowel-habits.pdf U.S. Department of Agriculture, Agricultural Research Service. (2019). FoodData Central. Retrieved from fdc.nal.usda.gov. Sanders, M.E. et al. (2018). Probiotics for human use. Nutrition Bulletin, 43, 212. Silva, C.A.G., & Motta, M.E.F.A. (2013). The use of abdominal muscle training, breathing exercises and abdominal massage to treat paediatric chronic functional constipation. Colorectal Disease. 15(5), 250-5. The ibs Network. (n.d.). Developing a good bowel habit. Retrieved January 21, 2021, from https://www.theibsnetwork.org/constipation/developing-a-good-bowel-habit/ Tong, P. C. (2017). Constipation and Faecal Incontinence. In Kong, T. K. (Ed.), The Hong Kong Geriatrics Society: Curriculum in geriatric medicine (2nd ed.) (pp.201-209). Hong Kong: Hong Kong Academy of Medicine Press. Tuck. C. et al. (2018). Fermentable short chain carbohydrate (FODMAP) content of common plant-based foods and processed foods suitable for vegetarian- and vegan-based eating patterns. Journal of Human Nutrition and Dietetics, 31(3), 422-35. Turan, N., & Aşt, T.A. (2016). The effect of abdominal massage on constipation and quality of life. Gastroenterology Nursing, 39(1), 48-59. Wu, J. C. Y., Chan, A. O. O., Cheung, T. K., Kwan, A. C. P., Leung, V. K. S., Sze, W. C., & Tan, V. P. Y. (2019). Consensus statements on diagnosis and management of chronic idiopathic constipation in adults in Hong Kong. Hong Kong Medical Journal, 25(2), 142-148. https://doi.org/10.12809/hkmj187692 Wu, T.J., Wei, T.S., Chou, Y.H., Yang, C.P., Wu, C.L., Chen, Y.C., & Liu, S.Y. (2012). Whole‐body vibration for functional constipation: a single‐centre, single‐blinded, randomized controlled trial. Colorectal Disease, 14,779-85. Yao, C.K. et al. (2014). Dietary sorbitol and mannitol: food content and distinct absorption patterns between healthy individuals and patients with irritable bowel syndrome. Journal of Human Nutrition and Dietetics, 27(2), 263-75. Yıldırım, D., Gülbeyaz, C., & Gül Köknel, T. (2019). The efficacy of abdominal massage in managing opioid-induced constipation. European Journal of Oncology Nursing, 41, 110-9. Zhang, R. et al. (2015). The Difference in nutrient intakes between Chinese and Mediterranean, Japanese and American Diets. Nutrients, 7(6), 4661–88. Zhao, Y., & Yu, Y.B. (2016). Intestinal microbiota and chronic constipation. Springerplus, 5(1), 1130. 〈中醫基礎理論 第36講 氣與精、津液的關係 經絡的概念和經絡系統〉。2020年12月30日,取自https://www.theqi.com/cmed/class/class5/c36.html 甘君學(2020年12月28日)。 〈養生帖:按摩+按穴 防治秋冬便秘〉。《明報》。取自 杜麗萍(2016年1月5日)。〈中醫如何治療便秘?〉。《每日頭條》。取自https://kknews.cc/health/29vq5jr.html 周仲瑛(2019)。 《中醫內科學第2版 》。 北京:人民衛生出版社。 周珈瑩(2017年5月5日)。〈中醫防治老年性便秘〉。《房協長者通》。取自https://hkhsolder adult.com/tc/health/medicine/485 林洋(2020年7月27日)。〈【便秘穴位】助腸道蠕動7大穴位按幾耐最好?按完再揉肚效果更佳〉。《香港01》。取自 張偉文(2011年2月1日)。〈老人排便困難是罹患大腸癌、腦中風的高危險群〉。 《大紀元》。取自 Chapter 5
Management of Constipation in Long-Term Care Settings Why institutionalized older adults are more prone to constipation? Constipation is the most common defaecatory disorders seen in older adults. This is particularly prevalent among older patients in hospital and long-term care (LTC) setting. For hospitalized older patient, the reasons are multiple, including medical conditions, drug sides effects, dehydration, immobility, and poor oral intake. Constipation in hospitalized older adults is indeed associated with adverse events, prolonged stay, and increased medical cost. Older adults living in LTC homes are vulnerable and reliance on high level of assistance, specialist nursing and medical care. They are suffering from multiple comorbidities and taking numerous medications. Most of older adults living in LTC homes are chairbound or bedridden. Deconditioning, dehydration, limited mobility and at risks of malnutrition that make them more prone to constipation. Constipation causes abdominal discomfort or pain. In severe cases, it can cause faecal impaction, urinary incontinence or retention, bowel obstruction, bowel perforation and suffering. The consequence of constipation has significant impacts on physical, psychosocial, quality of life and health expenditure among older adults and caregivers. Prevalence of constipation • In general population worldwide ranges from 0.7-79%. • Institutionalized older adults are more likely suffering from constipation. • The prevalence of constipation increases with age. • Women are more likely suffering from constipation than men. Tong (2017)
In Hong Kong, the Population Health Survey 2014-2015 from Department of Health reported: • Increased prevalence of acute constipation • Aged 15 to 64 range from 1.6% to 3.1% • Aged >65 range from 4.2% to 7.9% • (Aged 65-74: 4.4%; Aged 75-84:7.9%; Aged>85 12%) Factors contributing to constipation Factors contributing to constipation The “Ds” refer to the varies factors associated with constipation including: • Dementia • Depression • Degenerative disease • Drugs side effects • Decreased dietary intake especially fiber • Dehydration • Decreased mobility or immobility • Defaecatory dysfunction Medical conditions associated with constipation 
What are the unique issues related to constipation in LTC settings? The unique issues related to constipation in LTC settings • High prevalence of dementia • Co-morbidities • Polypharmacy • Inadequate food and fluid intake • Environmental limitations • Multifactorial • More severe complications • High usage of laxatives Older adults living in LTC homes are old and frail. They suffer from multiple comorbidities. According to the Census and Statistics Department (2009), 97.1% of residents had one and above chronic illnesses and 57.2% of them needed 1 to 4 kinds of drug treatment. About 42.5% needed 5 types and more medications. Their medical conditions and drug side effects add together to increase the chance of constipation in LTC residents. Institutionalized older adults are vulnerable group that require a higher level of care assistance, nursing and medical care. Mostly, impaired mobility in chairbound or bedridden residents are more prone to constipation. Studies found that laxatives use is high in LTC settings. High prevalence of dementia The increasing number of dementia cases in LTC requires special nursing care attention. Dementia is a clinical syndrome leading to cognitive impairment. People with dementia are having difficulty in communication and self-care in their daily lives. They deserve greater nursing care support to address their special needs, bowel and bladder issues in particular. Dementia with constipation • Neglect • Under-reporting • Difficult to monitor • Inadequate food and fluid intake • Dependence for toileting • Impaired rectal sensation • Atypical presentations Atypical presentation of constipation is commonly found as they are unable to express their discomfort and needs. They may have behaviour problem duo to their inability to voice out this problem. Health care professionals must understand the meaning behind their behaviour and pay special attention to the atypical presentation to detect any clinical sign and symptoms of health problem. Atypical Presentation of Constipation in LTC Residents with Dementia • Anorexia • Abdominal discomfort/distension • Urinary and/or faecal incontinence • Behavioral changes • Functional decline • Delirium Polypharmacy • Comorbidities • 92.7% taking routine medications • 57.2% taking 1 to 4 kinds mediations • 42.5% taking 5 types and more medications. • Drug side effects cause constipation • Drugs may have cumulative anticholinergic effects (Census and Statistics Department, 2009) Medications cause constipation • Anticholinergics (psychotropics, antihistamines, anti-parkinsonian drugs, antiemetics, antimuscarinics for incontinence) • Iron supplements • Calcium supplements • Opiates • Calcium channel blockers • NSAIDS • Diuretics Inadequate food and fluid intake • Feeding self-care deficits • Tooth decay • Minimal fiber intake • Altered thirst sensation • Medication side effects e.g. diuretics Impaired Mobility • Dependence for toileting • Deconditioning • Chairbound or bedridden • Low physical activity • Decreased ability to generate abdominal force Environmental limitations • Communal living environment • Lack of privacy, shared bathroom • Rarely provide a stress-free and private bathroom • Staff too busy in assisting toileting • Continence devices not comfortable Cause of Constipation in LTC is Multifactorial • Complex medical condition • Comorbidities • Polypharmacy • Poor dietary intake • Immobility Pathophysiology of chronic constipation (Andrews & Storr, 2011) 
Primary causes are intrinsic problems of colonic or anorectal function, whereas secondary causes are related to organic disease, systemic diseases or medications. The consequence of constipation can be critical and impact on physical, psychological health and well-being. What are the roles of nurses in managing constipation? The roles of nurses in managing constipation • Care Coordinator • Collaborate with team to plan for patient care • Professional Caregivers • Perform assessment and diagnostic tests • Record medical history and symptoms • Monitor patient health condition • Administer medications and treatments • Monitor medication side effects • Advocator • Advocate for health and well-being • Educator • Disease education to manage the health problem Nurses are playing important roles in managing constipation. Older adults living in hospital or LTC settings are having moderate to severe physical or cognitive problems. Most of them are dependent and require nurses to provide personal and nursing care for activities of daily livings. Nurses should strengthen their roles in caring of institutionalized older adults to meet their individual needs. Nursing process with a systematic approach should be applied including assessment, diagnosis, outcomes identification, planning, implementation, and outcome evaluation. Using the fundamental principles of critical thinking and client-centered approaches with evidence-based practice are important to ensure the care quality in managing constipation. How to assess constipation? Assessment of constipation Details assessment of constipation is discussed in the Chapter 2: Assessment of Constipation which included: • History taking • Red flags • Clinical assessment • Further Investigations Effective constipation management requires thorough assessment. Professional communication skill is essential to collect sufficient information for diagnosis. Defaecation problem is an embarrassing issue that older adults may be reluctance to talk about this. A non-judgmental and empathetic professional manner is recommended. Patient particular information can be collected from caregivers if patient has any communication problem such as dementia. Nurses can also perform the physical assessment such as palpation of abdominal mass and auscultation of bowel sounds to detect any abnormality and make the diagnosis or referral. Investigate any Red Flags that indicate something more serious. Refer to Chapter 2 Assessment of Constipation for details. How to assess constipation? (2) In Hong Kong, daily assessment of bowel movement is common practice in LTC settings. The assessment form included the following items: frequency of bowel movements, time of bowel movement, amount of stool, stool consistency and use of laxatives. A stool diary is useful to record the defaecation pattern. Bristol Stool Form Scale should be used to facilitate the mutual understanding and communication of the stool form. If the daily monitoring is delegated to the frontline care workers, nurses should provide sufficient education and monitor the care quality. If self-reporting is applied, nurses should provide education to make sure patient and family caregivers understand how to record the stool diary correctly. Refer to Chapter 1.3 “What should the stool look like?” for Bristol Stool Form Scale. How to manage and prevent constipation? For mild to moderate constipation, maintain healthy lifestyle is essential to prevent constipation. Lifestyle modification including increased fluid intake, increased physical activity, regular toileting schedule, and intake of dietary fiber and probiotic products are recommended to prevent and treat constipation. Details refer to Chapter 4: Lifestyles modification to prevent constipation and Exercise videos Pharmacological intervention is initiated if non-pharmacological intervention is not successful. Different kinds of laxatives would be considered to treat constipation. In general, laxatives can be classified into four main categories: 1. Bulk-forming laxatives 2. Osmotic laxatives 3. Stimulant laxatives 4. Stool softeners Single or combination of laxatives would be prescribed according to different types of constipation. However, overuse of laxatives should be avoided to prevent severer complications. Details refer to Chapter 4.8 Pharmacological Intervention for Constipation How to manage and prevent constipation? (2) Bowel Management Programme Bowel management may be neglected in our daily clinical practice. However, it can cause severer complications if unattended. Systematic management approach is recommended to prevent and treat constipation. Sit and her team in the ICU at Tuen Mun Hospital developed a bowel management guideline to guide the clinical practice in management of constipation. The bowel management programme was implemented and reported effectively in improving constipation and diarrhea events as well as patients’ health outcomes. (Sit, 2013) Link to view: http://www.hkaccn.org/newsletter/news201308.pdf
Link to view: https://www.jabfm.org/content/24/4/436/tab-figures-data
Link: https://www.aafp.org/afp/2015/0915/p500.html#afp20150915p500-f1 How to manage and prevent constipation? (3) Factors affecting nurses to preform constipation management • Busy working schedule • Lack of case conferences • Lack of staff resources • Lack of educational opportunities (Takaoka, 2020) Bowel care should be put in the priority of care. Education and management support for healthcare professionals is important to ensure effective clinical practice in constipation management. A clinical guideline according to different LTC settings is recommended to ensure quality management of constipation for older adults. This will facilitate professional reflective practice concerning the management of constipation to meet the individual care needs of institutionalized older adults for better health outcomes. - End of Chapter 5- Reference Andrews, C. N., & Storr, M. (2011). The pathophysiology of chronic constipation. Canadian journal of gastroenterology, 25 Suppl B, 16B–21B. Census and Statistics Department, HKSAR Government. (2009). Thematic household survey report No. 40.socio-demographic profile, health status and self-care capability of older persons. Retrieved from https://www.statistics.gov.hk/pub/B11302402009XXXXB0100.pdf Department of Health. (2017). Population Health Survey 2014-2015. Retrieved from https://www.chp.gov.hk/en/static/51256.html International Longevity Centre-UK, & Norgine. (2013). The burden of constipation in our ageing population working towards better solutions. Retrieved from https://ilcuk.org.uk/wp-content/uploads/2018/11/Burden-of-constipation-report.pdf Leung, L., Riutta, T., Kotecha, J., & Rosser, W. (2011). Chronic Constipation: An Evidence-Based Review. The Journal of the American Board of Family Medicine, 24(4), 436-451. DOI: 10.3122/jabfm.2011.04.100272 Lundberg, V., Boström, A. M., Gottberg, K., Konradsen, H. (2020). Healthcare professionals' experiences of assessing, treating and preventing constipation among older patients during hospitalization: an interview study. Journal of Multidisciplinary Healthcare, 13, 1573-1582. DOI https://doi.org/10.2147/JMDH.S277727 Medical Arts Pharmacy Newsletter. June 2018. Managing chronic constipation in long-term care with a focus of myths and facts. Retrieved from https://www.medicalartspharmacy.ca/wp-content/uploads/2018/05/Newsletter-MAP-June2018.pdf Morley, J., Tolson, D., Ouslander, J. G., Vellas, B. (2013). Nursing home care. McGraw Hill Professional. Mounsey, A., Raleigh, M., Wilson, A. (2015). Management of Constipation in Older Adults. American of Family Physician, 92(6), 500-504. Takaoka, M., Igarashi, A., Futami, A. et al. (2020). Management of constipation in long-term care hospitals and its ward manager and organization factors. BMC Nursing, 19, 5. https://doi.org/10.1186/s12912-020-0398-z Tong, P. C. (2017). Constipation and Faecal Incontinence. In Kong, T. K. (Ed.), The Hong Kong Geriatrics Society: Curriculum in geriatric medicine (2nd ed.) (pp.201-209). Hong Kong: Hong Kong Academy of Medicine Press. Wu, J. C. Y., Chan, A. O. O., Cheung, T. K., Kwan, A. C. P., Leung, V. K. S., Sze, W. C., & Tan, V. P. Y. (2019). Consensus statements on diagnosis and management of chronic idiopathic constipation in adults in Hong Kong. Hong Kong Medical Journal, 25(2), 142-148. https://doi.org/10.12809/hkmj187692 Quiz, feedback and certificate
Reference Link Reference Link
· Cadenza Public Seminars
· Drug office, Department of Health
· Hong Kong Pharmaceutical Care Foundation
· CUHK The Nethersole School of Nursing,The Nethersole Nursing Practice Research Unit (NNPRU)
· Centre for Health Protection
· Elderly Health Service, Department of Health
· Medicine online
Relevant Cadenza Training Materials Disclaimer The videos in this course provide information for educational purposes only. The videos do not provide medical recommendations or diagnoses and are not substitutes for medical advice. It is crucial that you talk with your healthcare providers to discuss any questions you may have and seek them for medical advice, before you make any medical decisions. As the videos are only for educational purposes, we will not be responsible for any decisions you will make or consequences you will have based on the information they provide. |
|
About Us About CADENZA About CADENZA e-Tools for Elder Care Contact Us |
|
e-Tools Online Courses Elder Care Training Courses For Professionals Elder Care Tips For Public |
|
|
App iHealth Screen |
|
© 2022 Jockey Club CADENZA e-Tools for Elder Care. All Rights Reserved.
|
Back to top ▲ |