In advanced endoscopy, what classifies as a “difficult case”? The answer is, of course, different for each advanced or interventional endoscopist. Some might define the level of “difficulty” based on the endoscopic technical aspects, some consider the procedure complications, while some reflect on the emotional engagement during the treatment of any particular case. ‘What is the most difficult case of advanced endoscopy you have ever encountered? What have you learned from it?’ In this case series, we have invited prominent advanced endoscopists in Hong Kong to share their stories with us.

In my memory, the most difficult case was one where I could not alter the patient’s disease course in spite of my best effort coupled with the most advanced technology in endoscopy.
It is one of those moments when I was forced to accept the fragility of life and limitations of advanced technology in treating human beings and diseases.
RAYMOND TANG
Clinical Professional Consultant,
Institute of Digestive Disease
Deputy Director of Endoscopy Centre,
Prince of Wales Hospital
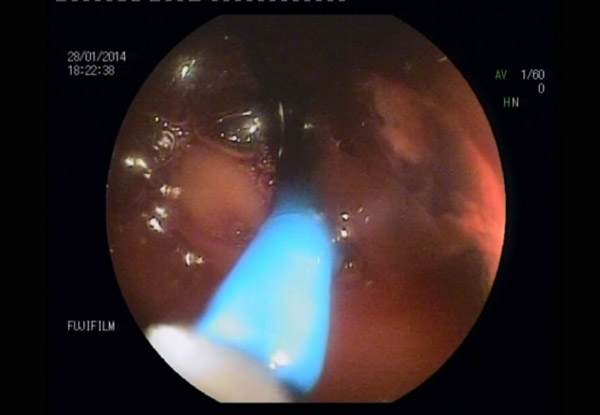
I often think of my patient, CL, who passed away a few years ago from complications of IgG4 disease, when I am asked to describe some of the most difficult and challenging cases during my practice in advanced endoscopy. CL was a gentleman in his 70s when he first consulted me for the management of his recurrent IgG4 disease of the hepatobiliary system. IgG4 disease is an autoimmune condition that often affects the lymph nodes, biliary tree, pancreas and liver. However, when CL first presented with symptoms of the IgG4 disease (bile duct narrowing causing obstruction) more than 15 years ago, doctors’ understanding of this rare autoimmune condition was limited so he was thought to have bile duct cancer and was subsequently managed with surgical resection and reconstruction of the biliary system and small intestine. The resected tissue specimen finally revealed the actual disease entity –IgG4 disease, instead of cancer. His IgG4 disease was in remission until several years ago when he presented with recurrent episodes of obscure GI bleeding and cholangitis, leading to a GI consultation. Because of his surgically altered anatomy, we performed balloon enteroscopy assisted ERCP, a technically demanding endoscopic procedure, which finally helped us to solve the mystery. What CL actually had was recurrent inflammation of his biliary-intestinal anastomosis caused by active IgG4 disease, resulting in bleeding and biliary obstruction. Despite solving one important mystery by the use of advanced technology, his subsequent clinical management was still full of challenges. For example, the need for multiple medications including immunosuppressive medications and a delicate balance between adequate control of his autoimmune disease, but without putting him at risks for recurrent infectious complications and bleeding in an elderly patient with multiple comorbidities.
It is common that many patients may be aggravated with confusion and fear by the diagnosis of a rare chronic condition without a definitive cure, leading to frequent clinic visits or hospitalization. Some might even sink into denial. In contrast, CL’s calmness and optimism about his condition surprised me during my care for him. During his multiple hospitalizations, he would tell the treatment team that he has looked up his condition on the internet and appreciated what the team had done for him and his condition. Unfortunately, his disease condition gradually worsened despite adequate treatment, leading to increasingly frequent admissions for the management of disease related complications. I was saddened to see how his condition deteriorated over time despite offering him our best medical treatment and the most advanced endoscopy. CL eventually passed away due to infectious complications after fighting this rare illness for many years.
CL was my first IgG4 disease patient who passed away (most of my IgG4 patients are younger and less sick). This case also qualified as one of my most difficult cases in advanced endoscopy. Perhaps, many of my colleagues would remember CL because of all the difficult endoscopic procedures our team had done together for him. I remembered CL because of his cheerfulness and optimism in fighting his rare disease condition and complications together.
The term “difficult case” may have a different meaning for different advanced endoscopists. But for me, as I have illustrated with CL’s case, the most difficult aspect of advanced endoscopy was to lose a long term patient and a long term friend who had worked together with me all these years in his disease treatment. I dedicate this article to CL.