-

Colon - Fecal immunochemical test
Fecal immunochemical test
The scary thing of colorectal cancer is that there are often no obvious symptoms in early onset stage. And when symptoms appear, disease is already proceed to late stage. Regular screening can help early diagnosis before it is too late to cure. There may be cases of bleeding occur if people are suffering from colorectal polyps, tumors or inflammation and other abnormalities and the blood may be mixed with stool and passed out. However, due to a very small amount of bleeding, patients are difficult to aware. Fecal occult blood test is capable of detecting if there is visually undetectable blood in stool and so it is called "occult blood" test. Research indicates that regular annual fecal occult blood tests can detect if there is any abnormal bleeding (positive result) happened in colon, as a result, incidence and mortality of colorectal cancer can be reduced effectively. Our center provides new type of fecal occult blood test which requires just a stool sample and no need to restrict diet beforehand. Subject have to follow the instructions to collect a small amount of stool sample and then return it to the center for testing. The process is simple and convenient.

- Colon Capsule Endoscopy
Colon Capsule Endoscopy
The colon capsule endoscopy is a new endoscopic technique. Through a pill-sized capsule with cameras on both ends and a small data recorder, medical staff can view the inner wall of the colon This examination time is usually within 9 hours, it will then be naturally passed out during bowel opening. This examination is accurate, simple, safe, low-invasive and also require no sedatives. Subjects’ discomfort and inconvenience can be effectively minimized.
In order to ensure a clear image of the inner wall of colon, subjects have to follow the instructions to have bowel preparation in advance.

- Colonoscopy / Sigmoidoscopy
Colonoscopy / Sigmoidoscopy
What is A Colonoscopy?
A colonoscope is a flexible tube-like device with a camera for visual inspection of the colon (large intestine), which includes the rectum, sigmoid colon, descending colon, transverse colon, ascending colon, cecum and terminal ileum.
If a polyp is found during a colonoscopy, it will be removed, and sent for a pathology review. If other abnormalities are found, a biopsy can be taken and sent for pathology review.
When is a colonoscopy needed?
A colonoscopy can be performed for screening purposes or for diagnostic evaluation. A screening is for individuals who do not have symptoms and is used to remove polyps and/or detect early colorectal cancer (CRC). International guidelines recommend CRC screening, such as by colonoscopy, starting at 50 years old in general. CRC screening has been shown in multiple studies to reduce the risk of CRC, by removing polyps and preventing their progression to CRC.
High-risk patients, particularly those with a first degree relative (parents, siblings or children) with CRC, should be screened earlier at 40 years old. Recent research conducted at the Chinese University of Hong Kong has also shown that siblings of patients with high risk adenomas are also at a higher risk of developing polyps, and likely benefit from earlier screening.
A colonoscopy is also performed for diagnostic evaluation of symptoms such as rectal bleeding, changes in bowel movements, abdominal pain, tenesmus, unexplained weight loss and anaemia, which may be symptoms of CRC.
How to prepare for a colonoscopy?
Once a physician has recommended a colonoscopy, detailed preprocedural instructions, which include dietary restriction (low residue diet), a colon cleansing routine and use of prescribed medications, will be provided. The purpose of this preparation is to cleanse the colon to ensure a complete and accurate examination. It is important to follow these instructions closely. Patients are recommended to be accompanied by a family member or friend for their safety after bowel preparation.
What happens during a colonoscopy?
Prior to the examination, intravenous sedation will be administered to reduce patient discomfort and anxiety. The flexible colonoscope will then be introduced through the anus to start the examination, which usually takes approximately 30minutes to perform. If a polyp is found, the endoscopist can immediately remove it with forceps or a wire loop and send the specimen for pathology review. Colonoscopies are in general well tolerated, and there should be no pain with polypectomy.
What happens after your colonoscopy?
A report of the colonoscopy findings will be provided. (we will provide the full colonoscopy report after the exam finish, but patient need to wait for histology report, if any) If polyps or biopsies were taken during the colonoscopy, pathology results will be provided as soon as possible (normally within a few weeks). Patients can in general leave the endoscopy centre the same day and are recommended to be accompanied by family members or friends. Patients should avoid operating heavy machinery, driving or signing any important documents or contracts for the rest of the day.
What are the possible risks of a colonoscopy?
Colonoscopies by experienced endoscopists are in general well tolerated and safe. Risks of serious complications are less than 1 in 1000 chance, and include cardiopulmonary complications, perforation and bleeding, etc. If these events occur, admission for monitoring, further investigations and treatments will be prescribed per standard practice.
What is the cost of colonoscopy?
The price of colonoscopy will depend on whether there are any polyps, the number of polyps, and medication. Please contact our staff at 3505 4316 for further details or check out our homepage to see what we can do for your health.

- Colorectal cancer screening programme
Colorectal cancer screening programme
For those who were born between 1944-1970
(Starts from 1 Jan 2020)
Colorectal cancer screening programme is being organized by Department of Health with the purpose in conducting colorectal cancer screening to health eligible subjects. In response to such meaningful programme, our centre has joined the programme to provide the service. Subjects will first need to conduct the faecal immunochemical test (FIT) within the programme. If the result is positive, the subject can then choose to conduct colonoscopy provided by colorectal cancer screening programme as a follow up on a free-of-charge basis. If you would like to understand more on eligibility criteria, please click here.
DH Colorectal cancer screening programme procedures
- 1. Register Electronic Health Record Sharing System (click here )
- 2. Make appointment with Primary Care Doctors to register and get the FIT package
- 3. Collecting sample at home
- 4. Return the sample to designated venue
-
5.1. If the FIT results are negative, you may continue the test in 2 years and beware of colorectal cancer symptoms 5.2. If the FIT results are positive, you will be appointed to meet the doctor again and refer for colonoscopy
- Colon Assessment Public-Private Partnership Programme
Colon Assessment Public-Private Partnership Programme

Colon Assessment Public-Private Partnership Programme (Colon PPP)
To cope with the increasing needs of colonoscopy service, the Hospital Authority (HA) is now commencing Colon Assessment Public-Private Partnership Programme (Colon PPP). It is to subsidy eligible subjects to undergo colonoscopy in private sector, meanwhile, providing one more choice for patients. This can help the patients to receive colonoscopy and treatment as early as possible. If you are in the colonoscopy queue under hospitals of HA and your health condition is eligible for the programme, you may be invited by HA staff to join this programme. Our centre is one of the premises under this Colon PPP.
-

Esophagus and Stomach - Upper gastrointestinal endoscopy
Upper gastrointestinal endoscopy
What is upper gastrointestinal endoscope?
An upper gastrointestinal endoscope is a flexible fiber-optic which consists of a camera that can view the image of the oesophagus, stomach and duodenum.When to conduct an upper gastrointestinal endoscopy?
If anyone who encounter one of the colorectal cancer symptoms such as peptic ulcer disease or bleeding, black stool, stomach pain, oesophageal or gastric cancer, symptoms of indigestion, acid reflux or difficulty in swallowing, they should go for upper gastrointestinal endoscopy to check whether there is any abnormality such as ulcer or cancer.Preparation before upper gastrointestinal endoscopy
Prior to upper gastrointestinal endoscopy, a period of 6-hour fasting is needed. Patient should inform the medical staff of any major medical problems including diabetes, hypertension and pregnancy, and continue their medications as instructed. Patient should also provide information concerning the current medications used and any allergic history. Patients should avoid driving to attend the out-patient procedure appointment and also avoid heavy drinking, smoking or use of sedative before the procedure. All patients are recommended to be accompanied by family member or friend for their safety.How is the process of upper gastrointestinal endoscopy?
Prior to the examination, local anaesthetics would be sprayed to the throat of patient. A flexible colonoscope with a diameter of 0.9-1.2 cm will then be introduced by the endoscopist through the mouth to perform the examination. In general, the procedure would last for around 15 to 30 minutes. But according to complexity, the procedure time may be prolonged.Possible risks or complications of upper gastrointestinal endoscopy
During the upper gastrointestinal endoscopy, minor discomfort including nausea and distention discomfort of stomach is common. The local anaesthetics would keep the throat numb for approximately one hour which will lead to swallowing difficulty. Major complications including perforation, bleeding, cardiopulmonary complication, infection or acute intestinal obstruction may happen. In general, the complication risk is less than 1% but it varies depending on patients’ conditions. Complication rate would be higher in cases that require polypectomy, endoscopic hemostasis or other relevant procedures. When major complications arise, emergency surgical treatment may be needed and mortality may happen. Patient should consult the attending physician for more information before the endoscopic procedure.Care after upper gastrointestinal endoscopy
Patients should remain fasted until anaethesia has worn off which will last for approximately one hour. This prevents choking with food or fluid intake. If intravenous sedation is used, patients should avoid operating heavy machinery, driving or sign any contract for the rest of the day. On the other hand, if there is any abnormality or enquiry about the examination, patient should contact our centre during office hour for query. If there is severe abdominal pain or gastrointestinal bleeding, patient should go to the nearest “Accident and Emergency” immediately and to inform their staff that upper gastrointestinal endoscopy has been done.
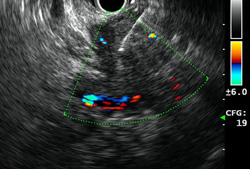
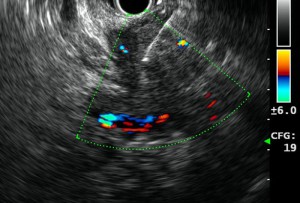
- Endoscopic ultrasound (EUS-gastric tract and stomach)
Endoscopic ultrasound (EUS-gastric tract and stomach)
What is an Endoscopic Ultrasound (EUS)?
Endoscopic ultrasound (EUS) is an endoscopic procedure for imaging of the upper gastrointestinal tract (oesophagus, stomach, and duodenum), and the pancreas to biliary system (bile ducts, gallbladder, and pancreas) using a flexible endoscope equipped with a small specialized ultrasound probe.
What are the reasons for undergoing an endoscopic ultrasound?
An endoscopic ultrasound may be recommended to patients who have or are suspected to have pancreatic disease in the pancreas or bile duct and can be both a diagnostic and therapeutic procedure. Usually an endoscopic ultrasound is recommended after abnormal test results or a patient experiences worrying abdominal pain symptoms thought to be related to the pancreas or bile duct.
Common conditions that can be evaluated by EUS are:
- gastrointestinal tract and pancreatic tumours,
- submucosal tumours,
- acute and chronic pancreatitis,
- pseudocysts and
- mediastinum lymph node.
How does an endoscopic ultrasound work?
Before undergoing EUS, patients are given sedation. A thin tube is inserted through the patient’s mouth and led down into the stomach. Once in the stomach, a small ultrasound probe at the tip of the tube emits soundwaves which produces a clear image of the desired area (such as the pancreas, digestive tract, or stomach). If masses or other signs of disease are found, a small biopsy will be taken for testing (with by EUS guided Fine Needle Aspiration (FNA).
Depending on the disease condition being evaluated, the duration of an endoscopic ultrasound examination usually lasts from 20 to 40 minutes.
Preparing for your endoscopic ultrasound.
A patient is asked to avoid eating and drinking for 8 hours before the procedure. Some medication should also be avoided prior to your appointment, so make sure to discuss this with your doctor. Following the procedure, it is advised that a family member or close friend should drive you home, that you avoid driving heavy machinery and signing important documents.
What are the risks of an endoscopic ultrasound?
EUS is generally considered a safe procedure when performed by an expert health team. However, like most medical procedures it carries a small risk of complications.
Risks may include:
- Tearing of the intestinal wall
- Bleeding
- Infection
- Pancreatitis (only a risk if fine-needle aspiration (EUS-FNA) of the pancreas is done)
How much does EUS cost?
The cost of the procedure depends on whether one or more samples need to be taken for testing, or if it is simply an imaging procedure. Please contact our staff at 3505 4316 for further details.
Also feel free to check out our homepage for other bowel-related queries.

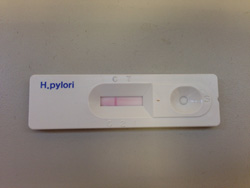
- Helicobacter Pylori Serology Test
Helicobacter Pylori Serology Test
Serology test is a simple, convenient and relatively cost-effective test for the detection of antibodies specific to Helicobacter Pylori in human serum, plasma or whole blood. It is often used for screening for Helicobacter Pylori infection. However, these tests are seldom be used to diagnose active infection or follow-up of eradication because of its relatively low accuracy. Unlike upper gastrointestinal endoscopy or urea breath test, fasting is not needed prior serology test.
- Urea Breath Test (UBT)
Urea Breath Test (UBT)
The urea breath test (UBT) is a non-invasive test for diagnosing the presence of a bacterium, Helicobacter pylori (H. pylori) in the stomach. H. pylori causes inflammation, ulcers, and atrophy of the stomach. The test also may be used for follow-up exam of H. pylori eradication treatment regime.
Comparing to OGD, urea breath test gives equally accurate result in terms of Helicobacter detection, while OGD provides additional information such as presence of inflammation or ulcer in the stomach.
- High resolution esophageal impedance manometry (HRIM)
High resolution esophageal impedance manometry (HRIM)
This test is indicated for suspected esophageal motility disorder (e.g. Achalasia), dysphagia, pre-operative assessment of anti-reflux surgery, non-cardiac chest pain.
HRIM studies the function of lower esophageal sphincter (LES) and esophageal motility. Local anesthetic will be given to patient and a catheter of 3mm diameter will be intubated through the patient’s nostril into the esophagus. After 10 minutes of resting, a sequence of swallowing tests (salt water or sometimes solid food) will be performed to access the motility of esophagus.


- Bravo® Wireless 24/48-hour esophageal pH monitoring
Bravo® Wireless 24/48-hour esophageal pH monitoring
Indication: Gastroesophageal reflux disease (GERD) with poor response to acid suppressive therapy, pre-operative assessment of anti-reflux surgery, non-cardiac chest pain
Procedure: The test studies the amount of acid reflux into the esophagus in 24 or 48 hours. Sedation will be given to the patient and a full diagnostic The Bravo capsule will be fixed to the esophagus with the help of endoscopy. The patient can be discharged after the procedure. The patient has to carry a wireless recorder during test (for 24 or 48 hours) and record the time of symptom onset, sleep and diet on a given diary. The patient will return the recorder and diary after 24 or 48 hours. The capsule will usually slough out spontaneously and passed out within 7-10 days. Compared to the traditional pH monitoring, Bravo wireless pH monitoring is more sensitive and better tolerated.

- 24-hour ambulatory esophageal impedance-pH monitoring
24-hour ambulatory esophageal impedance-pH monitoring
This test is indicated for patients who have gastroesophageal reflux disease (GERD) with poor response to acid suppressive therapy, pre-operative assessment of anti-reflux surgery, non-cardiac chest pain, liquid (acidic or non-acidic) regurgitation, repeated belching.
Local anesthetic will be given to patient and then a catheter of 1mm diameter will be intubated through the patient’s nostril into the esophagus. The patient will carry a portable recorder to which the catheter is connected. The patient can leave the hospital and resume normal activity during test, while recording the exact time of symptom onset, sleeping and diet on a given diary. The patient will come back to the hospital after 24 hours to have the catheter removed and to return the recorder and diary.


LiverLiver ExaminationLiver Examination
HBV DNA Test
HBV DNA quantification is an essential tool to assess the level viral replication in chronic hepatitis B. It is the standard investigation in patient selection for treatment as well as monitoring of treatment response and development of drug resistance. In our laboratory, we employ the TaqMan real-time polymerase chain reaction technology with the state-of-the-art ABI Prism system for measurement of HBV DNA. We use the Eurohep HBV standard to set the standard curve, which has a correlation coefficient routinely greater than 0.99. The linear range of HBV DNA measurement is from 100 to 109 copies/ml (20 to 2.0 x 108 IU/ml).
In order to ensure proper follow-up of the test results, all the requests require referral letters from doctors. To arrange an appointment for the test, please contact the Center for Liver Health during office hours to with a completed request form and a referral letter.
Drug-resistant variants of virus test
Use of anti-viral agents is associated with drug resistant mutations at the HBV polymerase gene. The emergence of drug resistance will lead to failure of treatment and worsening of liver disease. Early detection and confirmation of the drug resistant mutations will aid the clinical decision to modify the anti-viral regimes. In our laboratory, we perform polymerase chain reaction amplification and direct sequencing of the HBV polymerase gene to detect drug resistance. This assay has the advantage of detecting the key drug resistant mutations of different anti-viral drugs at the same time. In addition, compensatory mutations that may affect cross-resistance and viral replication fitness can also be detected.
In order to ensure proper follow-up of the test results, all the requests require referral letters from doctors. To arrange an appointment for the test, please contact the Center for Liver Health during office hours to with a completed request form and a referral letter.
FibroScan
Apart from liver stiffness measurement, Fibroscan has a new function to measure the controlled attenuation parameter (CAP). It is more convenient and bears a zero risk than the traditional assessment of liver fibrosis by liver biopsy. Technically, the operator will place a probe at the position of the liver where shear wave is emitted through the skin into the liver. At the same time, the probe will trace the velocity of the shear wave. The higher the velocity, the stiffness the liver. A stiffer liver usually reflects more severe liver fibrosis.
There are no obvious symptoms for fatty liver, liver fibrosis, liver cirrhosis and early stage hepatocellular carcinoma. Regular monitoring of liver fibrosis and cancer surveillance is recommended for early detection and treatment of these conditions, particularly among high risk patients.
To arrange an appointment for the investigation, please contact the Center for Liver Health during office hours.


Pancreas and bile duct systemEndoscopic ultrasound (EUS)Endoscopic ultrasound (EUS)
Endoscopic ultrasound (EUS) is an advanced endoscopic procedure specialized for the evaluation of various benign and malignant diseases involving the gastrointestinal tract and pancreatobiliary system using an ultrasound probe equipped on a flexible endoscope. Depending on the disease condition being evaluated, an EUS procedure usually takes about 20 to 40 minutes. Common conditions that can benefit from EUS are listed below (Table 1).
With its high resolution imaging, EUS can provide important information for local staging in patients with suspected gastrointestinal or pancreatobiliary tumours. When histological diagnosis is needed, EUS guided Fine Needle Aspiration (EUS-FNA) is a valuable technique for specimen acquisition. In addition to diagnostic evaluation, EUS can also be therapeutic. For example, in patients with chronic pain from pancreatic cancer, EUS guided Celiac Plexus Neurolysis (EUS-CPN) can provide effective palliation of cancer related pain, improving quality of life.
- Upper gastrointestinal tract submucosal tumors

- Common bile duct (CBD) stone

- Pancreatitis
- Pancreatic cystic neoplasm

- Abnormal liver function tests or obstructive jaundice
- Staging of upper gastrointestinal tract cancer, pancreatic cancer, bile duct cancer
- EUS guided Fine Needle Aspiration for specimen acquisition of upper gastrointestinal tract cancer and pancreatobiliary cancer and pancreatobiliary cancer
- EUS guided Celiac Plexus Neurolysis for pancreatic cancer pain control
- Mediastinal lymph node evaluation for lung cancer staging
- Upper gastrointestinal tract submucosal tumors

Small BowelSmall Bowel Capsule EndoscopySmall Bowel Capsule Endoscopy
The small bowel capsule endoscopy is a new endoscopic technology. Through a pill-sized capsule with cameras on one end and a small data recorder, medical staff can view the inner wall of the small bowel Examination usually lasted for eight hours and it will then be naturally passed out during bowel opening. This examination is accurate, simple, safe, low-invasive and also require no sedatives. Subjects’ discomfort and inconvenience can be effectively minimized.




