Chronic kidney disease patients in a bind on disability allowance
By Jayce Lai & Vivienne Tsang
Bonnie Ho Oi-ying releases around two litres of fluid from her abdomen from the end of the catheter inserted into her stomach. She then takes out a pack of fresh cleansing solution and the same volume of fluid flows into her abdomen. The process, called peritoneal dialysis takes 45 minutes to complete and the 60-year-old has to go through it three times a day just to stay alive. Ho, was diagnosed with end stage renal disease (ESRD) in 1987.
Patients are diagnosed as having ESRD when their kidneys can only function at below 10 per cent of their normal capacity. This means they are unable to effectively filter out metabolic waste such as urea. Unless they are able to receive a successful kidney transplant, such patients have to rely on dialysis to remove the excessive and harmful build-up of metabolic waste.
More than 8,500 ESRD patients were under the care of public hospitals in Hong Kong in December 2014. Around 5,000 of them need dialysis treatment and, around 80 per cent of them perform peritoneal dialysis.
Some, like Ho perform the treatment at home. Before they can do so, they are required to undergo training with nurses so that they know how to minimise infection. There is no subsidy for the treatment and it costs around HK$1,500 a month.

A more sophisticated form of peritoneal dialysis relies on a machine to conduct the fluids exchange. Automated peritoneal dialysis (APD) saves a lot of time as it can be performed while the patient sleeps at night. However, APD costs HK$6,000 a month and is not a common treatment in Hong Kong.
Some patients are unable to undergo any form of peritoneal dialysis because of they have malfunctioning peritoneal cavities and they need to undergo hemodialysis in hospitals or dialysis centres. In these cases, a machine drains blood from the patients’ arm and filters the waste, returning the clean blood to the body. The whole process takes around five hours, and patients need treatment every three days. However, each treatment costs at least HK$1,200.
With limited resources in public hospitals, the number of patients the government subsidises to undergo hemodialysis stood at just 156 in December 2014.
As Ho’s peritoneal cavity still functions, she is not qualified to receive subsidised hemodialysis. She spends HK$2,000 every month on her treatment. Because of the time constraints this imposes, she can only look for part-time jobs. Even this is a challenge and when she injured her hand in 2009, she stopped working altogether. Ho applied for disability allowance, but her application was rejected.
Disability allowance is a benefit under the Social Security Allowance Scheme to help disabled people meet the special needs caused by their disabilities. Successful claimants are entitled to either HK$1,510 under the normal disability allowance or HK$3,020 under the higher disability allowance. Most ESRD patients who manage to claim the benefit receive the normal disability allowance.
In order to qualify, patients must have their applications approved by public doctors who have to fill in a medical assessment form saying they are satisfied the patient has lost “100 per cent of earning capacity” or has “any other conditions including visceral diseases resulting in total disablement”.
Ho says some doctors do not accept that ESRD patients have lost 100 per cent of earning capacity. “The doctors think that we have arms hands and legs … we’re invisibly disabled,” she adds. However, as the chairperson of the Renal Companion Association, the patients’ association of Queen Mary Hospital, she knows that some ESRD patients with similar symptoms do get the disability allowance. It all depends on the doctor’s interpretation of the assessment criteria and Ho thinks this is unfair.
Leung Ka-lau, the legislator representing the doctors, is aware of this issue and says doctors should not regard being able to work as contradicting the “100 per cent loss of earning capacity” requirement.
Leung points out that the checklist on the third page of the assessment form provides more guidelines for doctors. The checklist states that being unable to work in the original occupation due to visceral disability is equivalent to “100 per cent loss of earning capacity”. Since ESRD patients’ working ability is lowered due to kidney failure, Leung thinks that ESRD patients’ applications should be approved.
“The doctors fill in the forms by themselves,” Leung says. “[They] often don’t have enough time to read the third page.”
Leung sent a letter to doctors in December 2013, and reminded them that patients with severe disability, like ESRD patients, may be eligible for the allowance even though they are employed. However, Leung’s letter did not bring significant improvement. Many patients still fail in their applications for disability allowance.
Daniel Chan Tak-mao, the chief of the Nephrology Division of the University of Hong Kong, says he has not read Leung’s letter. Chan says doctors will only consider medical factors and whether the disability has caused the 100 per cent loss of working ability in assessing the applications.

Chan says the aim of dialysis treatment is to help patients to recover, and that receiving treatment is not equivalent to disability. While he says he understands that ESRD patients need to receive frequent dialysis treatments, and have difficulty in finding jobs due to this, he asks: “But is this a social factor or a medical factor? This is a grey area.”
He explains that some applications were approved because the patients suffer from other diseases, such as heart disease, in addition to kidney disease. He thinks these other conditions may justify their applications.
However, Chan concedes a doctor’s judgment is subjective, and the definitions in the form are unclear. “If your kidneys lose 70 per cent functioning capacity, is it equivalent to disability?” he asks.
Legislator Fernando Cheung Chiu-hung, who has been working on the issue with renal disease patients’ organisations, says some developed countries consider “disability” from both a medical perspective and a social one.
He understands that doctors may not have enough time to assess social factors and thinks a “multi-professional assessment would be more comprehensive.” He suggests that a panel, including doctors, social workers and therapists should be set up to assess an application.
In a meeting of the Panel on Welfare Services in the Legislative Council in 2006, the government said such a panel review would lengthen the time to process applications. Instead it stressed patients could appeal, and the Medical Assessment Board would reassess their applications.
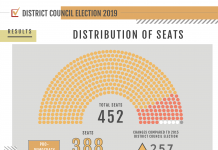
However, the board only consists of a doctor from the Hospital Authority and two representatives from the Hong Kong Medical Association. Its decisions are final and from 2013 to 2014, 67 appeal cases against medical decisions were successful, accounting for 25 per cent of 263 disability allowance appeals.
Cheung proposes a more immediate solution to the issue. He says the government should follow the suggestion of the Office of the Ombudsman in 2009 to delete “100 per cent loss of earning capacity” as an eligibility criterion. Cheung says as the policy objective of the disability allowance is simply to help patients meet the special needs caused by their disability, ESRD patients should be entitled to the allowance to subsidise the heavy cost of dialysis treatment.
Ma Chan-kwong, another ESRD patient and the chairman of Hong Ling Renal Club, also had his application for disability allowance rejected. However, as the 47-year-old has to take care of his mother, the Social Welfare Department (SWD) grants him Comprehensive Social Security Allowance (CSSA) payments of HK$7,000 per month.
Since his peritoneal cavity cannot function, Ma receives subsidised hemodialysis treatment and pays HK$300 each week. Despite getting CSSA, he finds it a struggle to make ends meet for himself and his mother. “No [social life] at all, unless I earn a bit more money from part-time jobs,” says Ma.
Ma was diagnosed with ESRD in 1990, but he kept on actively looking for jobs. As he has to visit the hospital three times a week for dialysis, he cannot work full-time. Even though he was willing to accept a lower salary, he still could not find employers who would take him on.
Later, Ma chose to be a part-time taxi driver. It is not just for the money that he insists on working. “I can’t just stay at home, and working can grant me a higher sense of achievement,” Ma explains. As Ma works part-time, the SWD deducts a certain amount of his allowance.
Joey Chan Pui-lam is the community relations manager of Alliance for the Renal Patients Mutual Help Association, whose members are the patients’ associations from nine public hospitals. She criticises the government for failing to provide support to help ESRD patients to find jobs.

Patients can seek help from non-governmental organisations, like the Hong Kong Society for Rehabilitation. But these organisations can only arrange training courses for patients, they cannot provide direct employment services.
Chan is also critical of the lack of government support for her association. The association organises frequent activities to promote knowledge and awareness of renal diseases in the community and encourages patients to become volunteers to enhance their social life. However, the SWD only provides them with HK$300,000 every two years.
“[The government] thinks that they have already done something by giving you the chance to have dialysis or see doctors,” says Chan.
She thinks the government’s policies are slanted towards other groups, such as the physically disabled. For instance, there are sheltered workshops with job opportunities for the disabled, as well as disability allowance and transport fare concessions.
Janet Hui is a member of Chan’s association, but she is luckier than many of her peers. Giving up on waiting for a kidney transplant in Hong Kong, she received one in Guangzhou in 1997. Now, she only needs to pay around HK$800 per month for anti-rejection medicines. Since the Mainland tightened regulations on organ donations and transplants in 2007, Hong Kong patients can no longer seek transplant operations there.
There are currently 1,965 ESRD patients waiting for kidney transplants in Hong Kong. Yet the number who will receive the surgery every year is small, due to the shortage of donor kidneys. In 2014, only 79 patients received the surgery.
Except for some dietary restrictions, Hui now leads an ordinary life. “I can do more things I like, including travelling and voluntary services,” she says.
“Kidney transplant is the only way to stop receiving [dialysis] treatment, to allow me to live as an ordinary person,” says ESRD patient and taxi driver Ma Chan-kwong. The greatest wish of many ESRD patients, including Ma, is to live normal lives with jobs and social lives, but to achieve this they need more support from the government and the general public.
Edited by Macau Mak